Our personal plumbing system
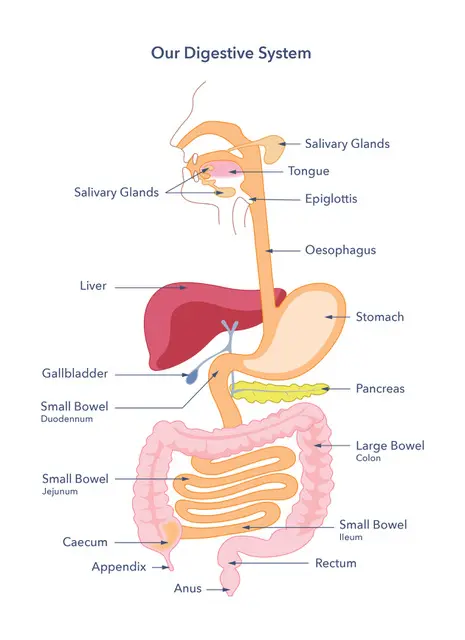 The gut is sometimes compared to a plumbing system: a long and twisting pipe with valves and fittings leading to fixtures. Your mouth chews food like a high-end food waste disposer and gulps it down into your oesophagus, or food pipe. Your stomach then adds liquid to the mixture and churns it not unlike a washing machine though admittedly you might not want clothes treated quite like that: your stomach adds acid to the mixture to help break down food.
The gut is sometimes compared to a plumbing system: a long and twisting pipe with valves and fittings leading to fixtures. Your mouth chews food like a high-end food waste disposer and gulps it down into your oesophagus, or food pipe. Your stomach then adds liquid to the mixture and churns it not unlike a washing machine though admittedly you might not want clothes treated quite like that: your stomach adds acid to the mixture to help break down food.
It is a good idea to eat slowly and chew your food well but just in case your stomach has two ‘valves’ to regulate how quickly food gets through it. One valve sits between the oesophagus and the stomach, the lower oesophageal sphincter, and the other ones sits between the stomach and the small intestine, the pyloric sphincter. A sphincter is a ring of muscle that can contract to close a hole and yes, you are right, there is a well-known sphincter at the far end of the gut but we will get to that one shortly.
What with all the chewing and churning and bathing in acid food doesn’t really look like food by the time your stomach squirts it out bit by bit past the pyloric sphincter into the small intestine, but that is nothing compared to what happens after that. Your small intestine is long and thin, the average length is 20 feet but it can vary quite a lot between individuals. The part of the small intestine closest to the stomach is called the duodenum, the middle bit is called the jejunum and the last bit is called the ileum – it is useful to know these names because the three parts have different jobs.
The duodenum curves gently as it leaves the stomach and in that curves fits snuggly an organ with a very important job in the digestion of food: the pancreas. You might know that the pancreas regulates your body’s sugar levels by producing insulin, the molecule that goes wrong in diabetes. However what you might not know is that the pancreas has another job. It produces another set of molecules called digestive enzymes, which break down the components that make up food into even smaller parts. When you look at a plate of spaghetti you see pasta, ham and cheese sauce; your pancreas sees carbohydrates, proteins and fats. It then produces digestive enzymes and pumps them into the duodenum, ready to meet the liquefied food that arrives from the stomach. These digestive enzymes act like specialised tiny scissors that cut starch, proteins and fats into much smaller components, small enough that they can be absorbed through the wall of your small intestine and pass into your blood. Most of these food components, or nutrients, are absorbed along the jejunum part of the small intestine.
Once the nutrients are in your blood supply these nutrients are taken to your liver. Your liver has many jobs but one of them is ensuring nutrients that arrive from your gut are managed properly so they can reach and nourish the rest of the body. Your pancreas helps with this job too, by releasing insulin into the blood – but that is another story so let’s get back to the gut.
Your small intestine has no problem absorbing small nutrients but it needs a bit of help taking in fats. To help, the liver produces a substance called bile. Bile is made in the liver and then temporarily stored in the gallbladder, a small sack sitting under the liver. When fat is present in the food, which is actually most of the time, the gallbladder secretes bile into the duodenum part of the small intestine. Bile binds itself to dollops of fat in the liquefied food and breaks them up into smaller droplets, a bit like when you add soap to oil. These smaller droplets can then be attacked by the pancreatic digestive enzymes responsible for breaking down fat into its smaller components. Bile is very useful – it even helps with the absorption of a few vitamins – but like most things in the body its job is best kept to the right place: the gut absorbs bile back into the blood and takes it back to the liver. This happens in the ileum, the last stage of the small intestine.
By the time your food is coming out of your small intestine it looks like a very thin and unappetising soup. However, there is someone waiting eagerly for this soup. The small intestine connects to the large bowel (or colon), a much shorter and wider section of the gut. The large bowel has some extremely important occupants: your gut bacteria. Gut bacteria are able to eat a food component we have not mentioned yet: fibre. Our small intestine is unable to absorb fibre from food, no matter how mashed up it might be, but our gut bacteria take to it with glee. Bacteria can sometimes eat other food components that might have slipped past your small intestine and strayed into your large bowel, such as starch, sugars or bits of protein, but generally they are keen on fibre. Or it seems that our ‘friendliest’ bacteria prefer fibre – there is still much we do not know about our gut neighbours, though this is an exciting area of research. In any case, our gut bacteria consume food components left in the large bowel while the bowel itself absorbs water and salts from the mixture. Slowly, over the course of a couple of days (give or take depending on the individual) the mixture gets thicker and drier until it forms into stools (faeces), which eventually reach the rectum and are excreted through the anus (the other sphincter we mentioned earlier!).
As you can see the process of food digestion and absorption along the gut is complex. Our internal plumbing is helped along by a complex network of blood vessels, part of the circulatory system. These blood vessels take nutrients from the gut to the rest of the body but they also keep the gut in good health. There is also a whole army of special cells and molecules, part of the immune system, whose jobs are to protect the body against any dangerous invaders. And importantly, there is a parallel electrical wiring along our gut, part of the nervous system, which helps to regulate the gut’s functions and movements.
All this complexity in the gut means that unfortunately things do sometimes go wrong. Things can go wrong with the way food moves along the gut, with how it’s broken down, with how nutrients are absorbed, or with how the digestive system interacts with other systems in the body such as the circulatory, nervous or immune system.
Starting at the top, swallowing can be impaired, causing coughing, choking and vomiting. This problem is known as dysphagia and can be caused by strokes and degenerative diseases that affect the nervous system, but also by damage to the oesophagus, for example by acid reflux, by eosinophilic oesophagitis (a condition where the immune system attacks the oesophagus causing inflammation and tissue damage) or by cancer.
Another condition that affects the oesophagus is called achalasia. Food normally moves down aided by a set of regular wave-like contractions of the muscles of the oesophagus in a motion called peristalsis. When food reaches the lower oesophageal sphincter (see above), the ring opens allowing food into the stomach. In achalasia the signals from the nervous system to the muscles do not work properly, disrupting peristalsis and sometimes preventing the lower oesophageal sphincter from opening, leading to food getting stuck in the oesophagus.
While food struggles to get down the oesophagus in some disorders, in other conditions the problem goes the other way around. The lower oesophageal sphincter has the extremely important job of stopping stomach contents sipping back up into the oesophagus. The lining of the stomach can tolerate the acid that is used to break down food, but the lining of the oesophagus is made from a different material and it can become irritated. Acid reflux (or Gastroesophageal Reflux Disease) is common and usually causes heartburn, that painful burn in the middle of the chest. Sometimes acid reflux can also damage the lining of the oesophagus in a condition called Barrett’s Oesophagus. In a small number of people this damage can lead to oesophageal cancer. Because of this increased risk people with Barrett’s Oesophagus are monitored for oesophageal cancer, to try to catch it early if it were to develop.
When food does eventually get into the stomach, sometimes it has a hard time getting out at the other end, past the pyloric sphincter (see above). In a condition called gastroparesis the nerves and muscles that control the normal movement of the stomach do not work properly. The stomach might not churn food sufficiently – or at all – or it might not empty it into the small intestine. This can cause an uncomfortable feeling of fullness, bloating, nausea and vomiting, as well as problems regulating blood sugars (by confusing the pancreas with promises of food that never arrives). Conversely, when the stomach offloads too much food too quickly into the small intestine, usually due to surgery or occasionally other causes, it can trigger a condition known as dumping syndrome.
The stomach is also the home of a well known digestive condition that has had a transformation in the last few decades: the peptic ulcer. Previously seen as caused by stress, the fortunate discovery of a type of bacteria called Helicobacter pylori by Australian researchers helped clarify how peptic ulcers develop. Now treated with antibiotics rather than milk of magnesia, peptic ulcers are not just extremely uncomfortable but can increase the risk of stomach cancer, when the ulcer is found in the stomach. Ulcers can also be found in the first part of the small intestine – the duodenum.
Moving on from the stomach we reach the small intestine. Another well known condition that affects this part of the gut is coeliac disease. The immune system of people with coeliac disease reacts inappropriately to a protein called gluten, which is present in wheat, barley and rye. This causes damage to the lining of the small intestine, hindering the absorption of nutrients and vitamins. There are other conditions, such as lactose intolerance, that can also stop the absorption of nutrients, though generally this is limited to one or a few specific nutrients.
The small intestine can also develop ulcers, adhesions (parts of the gut sticking to where they shouldn’t), blockages and motility problems including chronic intestinal pseudo-obstruction (a condition where no physical blockage of the gut is present but problems with the nerves and muscles of the gut lead to abnormal gut movement).
Problems with the pancreas such as pancreatitis, a serious and painful inflammation of that organ, can affect the breakdown and absorption of nutrients in the small intestine if the production of pancreatic enzymes is reduced (see above). Problems with the gallbladder can also have repercussions in the small intestine, affecting the absorption of fats (see above). The gallbladder can contain stones (gallstones) that can block the tube that connects the gallbladder to the small intestine, or the problem can be located in the valve, or sphincter, that regulates the passing of bile into the small intestine, as happens in the Biliary Sphincter Disorders. Sometimes the problem can extend to the large bowel in a condition called Bile Acid Diarrhoea, where bile acids are not reabsorbed by the small intestine and reach the large bowel, causing diarrhoea.
There are many conditions that affect the large bowel. Inflammatory Bowel Disease (IBD) is a group of diseases where the bowel appears inflamed and ulcerated. Crohn’s disease, one of these diseases, can actually affect the full length of the gut, from the mouth to the anus. Ulcerative colitis and microscopic colitis, two other types of IBD, are confined to the large bowel.
The large bowel can also develop distinct pouches called diverticula, in a common condition called diverticular disease. Often these pouches do not cause symptoms, or only mild discomfort, but they can occasionally become inflamed or infected, leading to complications, in what is called diverticulitis.
Another common condition of the large bowel is Irritable Bowel Syndrome (IBS). People with IBS experience cramp-like pain and abnormal bowel movements, such as diarrhoea, constipation, or sometimes both alternately. The causes of IBS are not clear though food poisoning or gastroenteritis seem to be common triggers of the condition.
The large bowel can also develop polyps, small growths on the wall of the bowel. Polyps are usually benign but a small number of them can go on to become bowel cancer, which is why bowel screening is so important.
There are many other diseases and conditions that affect the gut and the organs associated with it. The liver works hard to support our guts and our digestion but overeating and excess drinking will take their toll on that organ. People who are overweight or obese can develop metabolic dysfunction-associated fatty liver disease (MAFLD), a condition caused by a build up of fat in the liver. Excessive alcohol drinking can also damage the liver leading to alcohol-related liver disease (ARLD). Both MAFLD and ARLD can get progressively worse until they lead to liver cirrhosis, a scarring of the liver that stops the liver from working properly.
Cirrhosis can cause ascites, a build up of fluid within the abdomen. The abdomen can become so distended that people lose their appetite, become constipated, or feel indigestion, nausea or vomiting. Cirrhosis can also lead to liver cancer.
Our digestive system works hard to keep us well nourished and healthy, working with what we feed it. Its complexity means that there are many places where things can go wrong, which means identifying the cause of some digestive problems can be laborious and time consuming. Looking after our guts and keeping an eye on symptoms and signs can pay off.