Ulcerative Colitis
Download printable versionOverview
This factsheet helps to explain about ulcerative colitis, what causes it, the symptoms to be aware of and the treatments that are available.
Ulcerative colitis is a disease of the rectum and the large bowel, (otherwise known as the colon). Ulcerative colitis is thought to affect around 1 in 420 people, although it is becoming more common over time. The peak age of diagnosis is in people aged between 15-25 years old. There is a smaller peak occurring between the ages of 55 and 65 years old, but it can occur at any age.
INFLAMMATORY BOWEL DISEASE
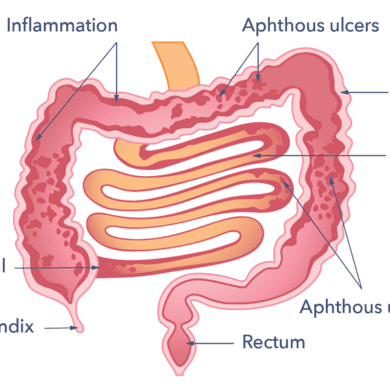
Ulcerative colitis (UC) is one of a group of conditions that are known as inflammatory bowel diseases, which also includes Crohn’s disease. The term ‘colitis’ means the lining of the large bowel (called the mucosa) has become inflamed (swollen, red and fragile), which means it can bleed at times. If this inflammation becomes severe enough ulcers (open painful sores) may form in the lining of the large bowel.
Causes
Causes of ulcerative colitis
We don’t yet know the cause of this condition. Most scientists and doctors now believe it is related to how the gut and body’s immune system react to bacteria in the bowel. In most people, the bacteria that live in the large bowel do not cause any damage and indeed can be quite useful. But, for people with ulcerative colitis the bacteria are not always as friendly.
The lining of the large bowel has a lot of immune cells. When the lining of the large bowel goes into battle with these bacteria, the result is inflammation. Inflammation can extend from the rectum (the last part of the large bowel) upwards into the colon. The distance the inflammation travels varies, sometimes inflammation involves the entire large bowel.
goes into battle with these bacteria, the result is inflammation. Inflammation can extend from the rectum (the last part of the large bowel) upwards into the colon. The distance the inflammation travels varies, sometimes inflammation involves the entire large bowel.
Research is under way to find out why people with ulcerative colitis appear to react badly to bacteria that don’t normally cause any harm in others. There is possibly a genetic (runs in families) link, plus an environmental link (what we eat, breathe, drink). These can then impact on how the immune system and the bowel bacteria interact with each other. A very specific environmental factor is yet to be discovered.
What does Ulcerative Colitis look like?
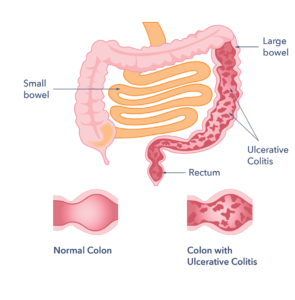
With UC there is a wide variation in the amount of inflammation from person to person. For people with mild inflammation, the bowel can look almost normal. But, when the inflammation is bad, the bowel can look very red and ulcerated. The inflammation can involve varying lengths of the bowel.
Ulcerative colitis usually affects the rectum. But in 1 in 20 people there is no rectal inflammation. This is called “rectal sparing”. Sometimes the inflammation affects the rectum only, this is called “proctitis”. Or it affects the left side of the large bowel, this is called left sided colitis. Sometimes it can be called pan (total) colitis, this is inflammation of the whole of the large bowel.
How is Ulcerative Colitis diagnosed?
The first steps to diagnosis include taking a full medical history. The doctor also looks at the person to check for pale skin and sores in the corners of the mouth, which can be signs of anaemia. Anaemia is when a person has low levels of iron in the blood which in this case is due to bleeding. The doctors will also gently examine the abdomen (belly) which includes feeling the abdomen for tenderness. Tenderness is a possible sign of inflammation.
For suspected UC further tests are carried out.
These will include:
Blood tests. These are to check both for anaemia and to ensure that other body organs such as the kidneys and liver are not affected by the problem in the bowel. They also measure the level of a sensitive protein, called C-reactive protein or CRP, which goes up if there is inflammation in the body. Another non-specific test of inflammation is called ESR. Generally, the greater the degree of anaemia and the higher the level of the CRP and ESR, the more severe the inflammation is likely to be.
liver are not affected by the problem in the bowel. They also measure the level of a sensitive protein, called C-reactive protein or CRP, which goes up if there is inflammation in the body. Another non-specific test of inflammation is called ESR. Generally, the greater the degree of anaemia and the higher the level of the CRP and ESR, the more severe the inflammation is likely to be.
Faecal microscopy, culture and sensitivity test and Clostridium difficile toxin tests. These are two poo tests which test the stool for any infections which may mimic the symptoms and signs of UC. It is very difficult to diagnose UC in the presence of an infection, so these tests need to be negative before UC can be diagnosed. If someone has already been diagnosed with UC, they are still tested for this if their symptoms get worse. People with UC can still get infections as well as their UC.
Faecal Calprotectin (FCP) test.  This poo test examines stools for signs of inflammation – high levels mean more severe inflammation. Whilst the FCP test can be raised with infections in the bowel and other unrelated conditions, it is most sensitive for people with IBD. Is also used to help check how a person is responding to treatment (whereby you would expect the FCP level to go back to normal levels).
This poo test examines stools for signs of inflammation – high levels mean more severe inflammation. Whilst the FCP test can be raised with infections in the bowel and other unrelated conditions, it is most sensitive for people with IBD. Is also used to help check how a person is responding to treatment (whereby you would expect the FCP level to go back to normal levels).
Abdominal x-ray. If the inflammation in the bowel is very severe, the bowel can become enlarged and at risk of perforating. If a doctor is concerned that this situation is developing a plain abdominal x-ray may be needed. Only rarely will a CT scan be requested.
One of the most important investigations is to look at the lining of the large bowel. This is done using a tube fitting with a camera which passed into the bowel via the anus. There are two types of investigations used for ulcerative colitis:
Sigmoidoscopy. This investigation only views the rectum and left-hand side of the large bowel. People will receive an enema to clear the bowel before the procedure. In most initial presentations of UC, a flexible sigmoidoscopy has been performed leading to that diagnosis.
Colonoscopy. This is a flexible tube, long enough to pass through your back passage and along the whole length of the bowel. A colonoscopy will confirm the diagnosis of ulcerative colitis. But it also provides information on the extent and severity of inflammation in the bowel. People follow a special diet and take laxatives before the colonoscopy. This is to ensure the bowel is empty. The person will be offered sedation and pain relief to minimise any discomfort.
the extent and severity of inflammation in the bowel. People follow a special diet and take laxatives before the colonoscopy. This is to ensure the bowel is empty. The person will be offered sedation and pain relief to minimise any discomfort.
For the sigmoidoscopy, tiny samples of the bowel lining (biopsies) may be taken. With the colonoscopy biopsies are likely to be taken. After the procedure has finished, the biopsies are looked at under a microscope. They are used to confirm the diagnosis.
How can Ulcerative Colitis affect you?
Ulcerative colitis varies from person to person. In some people the condition does not have much of an impact on daily life but in others, people can experience a lower quality of life.
Symptoms
The three most common symptoms are:
- Diarrhoea.
- Bleeding, or passing mucus (white jelly), from the back passage.
- Pain in the belly (abdomen).
Symptoms do differ from one person to the next, so many people may not have all three of these together. For example, some people may notice that they pass blood when they open their bowels. Others may not have diarrhoea but feel rather constipated. Symptoms may depend on how much of the large bowel is affected by the disease.
 For some people, the symptoms can be an annoyance but may be bearable. For others, the condition can interfere with day-to-day life. This can become organized around visits to the toilet. The urgency in which some people need the toilet can also be very upsetting. As symptoms are often at their worst in the morning, this can mean the start of the day can be quite an ordeal. Some people pass considerable quantities of mucus when they open their bowels. Others can be troubled by wind.
For some people, the symptoms can be an annoyance but may be bearable. For others, the condition can interfere with day-to-day life. This can become organized around visits to the toilet. The urgency in which some people need the toilet can also be very upsetting. As symptoms are often at their worst in the morning, this can mean the start of the day can be quite an ordeal. Some people pass considerable quantities of mucus when they open their bowels. Others can be troubled by wind.
Many people feel tired and not their usual self and they (or their family and friends) notice mood changes. For some people there are symptoms outside the abdomen. Symptoms outside the intestines are called extra- intestinal. Examples are sore eyes, painful joints, skin rashes and unexplained weight loss. Weight loss is a feature of severe disease. Symptoms outside the abdomen affect more designated females at birth than those designated males at birth.
Will Ulcerative Colitis affect me over time?
The effects of ulcerative colitis vary from person to person. The reason for variation is the nature and severity of their disease. The condition when treated may not have much impact on daily life, the ability to work or to enjoy an active social life. But ulcerative colitis does take some getting used to.
During the active disease stage, diarrhoea and abdominal pain often need the person to take time away from work or college. This can make it difficult to cope going out or even being at home. Mostly treatment makes the symptoms better within days or weeks. So normal quality of life can be restored.
diarrhoea and abdominal pain often need the person to take time away from work or college. This can make it difficult to cope going out or even being at home. Mostly treatment makes the symptoms better within days or weeks. So normal quality of life can be restored.
However, severe cases of ulcerative colitis can have a more significant impact on people’s lives. This can be due to a weaker response to treatment. This makes symptom-free remission difficult to achieve and can involve frequent flare-ups. Please see support section for further information about what is available to help.
Complications
A small number of people have complications that relate to ulcerative colitis in their skin, eyes, joints or liver. You will be checked, to see if any of these complications do develop so that they can be treated.
People with ulcerative colitis have an increased risk of getting bowel cancer. The highest risk being in those with pan ulcerative colitis who have had uncontrolled disease for a number of decades, or those with UC and a liver condition called primary sclerosing cholangitis (PSC). Your doctor will keep an eye on your bowel at regular intervals by performing a colonoscopy. This is to detect changes in the lining of the bowel at a stage well before any cancer has developed.
Treatment
What treatment is available for ulcerative colitis?
There are two main stages to your treatment. The first is to bring your condition under control (or induce remission). The second is long term management of your condition to keep it under control and avoid it returning (relapse). This is called maintaining remission. There is currently no cure for ulcerative colitis.
Induction of Remission
The medicine necessary to do this depends on the severity of your symptoms. The method of medicine delivery will also depend on the severity of symptoms. For proctitis, the doctor may recommend a medicine that you need to insert into the rectum, through the back passage. The thought of this can be unpleasant but this means the treatment is applied to the inflamed part of the bowel.
also depend on the severity of symptoms. For proctitis, the doctor may recommend a medicine that you need to insert into the rectum, through the back passage. The thought of this can be unpleasant but this means the treatment is applied to the inflamed part of the bowel.
Treatment can be given as suppositories or as enemas. Enemas can also be useful if the disease involves more of the large bowel. If the inflammation in the bowel is severe enough or is extensive in the bowel, it is also likely that you will be prescribed:
- Tablets to take by mouth.
- Intravenously (IV; medicines that go into the vein)
- Subcutaneously (S/C; medicines that are injected into the skin).
Medicines:
- Anti-inflammatory medicines. These include aminosalicylates. Aminosalicylates are also known as mesalazine (Octasa, Pentasa and Mezavant). These come in rectal and oral forms and may reduce risk of bowel cancer. Often peoples with UC will be asked to take both oral and rectal medicines at the same time.
- Steroids. If the inflammation is more severe then steroids may be used. They are given either in a tablet
 form or intravenously, in hospital if necessary. Your doctor will choose the preparation they feel is best for you. They are usually safe to use but doctors are reluctant for people to take these medicines long term as they can lead to weight gain, mood changes and acne in some people. This is because of the risk of side effects. But, most people do get better with these treatments as they do induce remission but should not be used to maintain remission.
form or intravenously, in hospital if necessary. Your doctor will choose the preparation they feel is best for you. They are usually safe to use but doctors are reluctant for people to take these medicines long term as they can lead to weight gain, mood changes and acne in some people. This is because of the risk of side effects. But, most people do get better with these treatments as they do induce remission but should not be used to maintain remission.
- Biologics. For people with moderate to severe inflammation biologic medicines are helpful as they block the proteins in the body (called cytokines) that can cause inflammation in UC. They get the disease under control (remission) and can also maintain remission over a long period of time. They can be given intravenously (IV) or subcutaneously (SC) which some medications initially being IV and then becoming SC after a few IV doses. Examples are infliximab (IV and SC), adalimumab (SC only), golimumab (SC), ustekinumab (IV then SC) and vedolizumab (IV and SC). If remission is achieved, these drugs can be continued in line with national guidance.
- New methods of giving infliximab and vedolizumab. These medicines can be given subcutaneously and have only recently been approved by NICE in the UK. These are pre-filled injection pens for injection under the skin. This reduces the need to attend infusion clinics. They can be given by the person with ulcerative colitis or their carers, in the community. This makes it easier for people to get on with their lives, but the dose will need to be given more often.
- Small molecule drugs. There are number of new oral medicines available now for the treatment of moderate to severe UC which reduce inflammation by blocking key pathways which cause inflammation in peoples with UC. These drugs are classified as:
- JAK (janus kinase) inhibitors: Examples include tofacitinib, filgotinib and upadacitinib.
- S1P (Sphingosine-1-phosphate) inhibitors: Examples include ozanimod.
In the next few years there are several other drugs in development that are going to be available for UC but are not available now such as mirikizumab.
Avoiding Relapse
Regular review by your doctor is important. This is to ensure that you are on the best possible treatment and that your symptoms are well controlled. A partnership between the person with UC, their GP and the specialist team can be very helpful. Any relapse will be treated using medicines as above. Treatment choice depends on the inflammation, the persons history and previous medicine responses. It is important to continue to take your medicine even if you feel well.
Hospital Admission
 Doctors try hard to control ulcerative colitis with drugs and medicines. Sometimes this might not work. The person may then have to be admitted to hospital for more intensive treatment and care. Usually this works well. Once the inflammation is back under control the person can go home with a maintenance treatment programme.
Doctors try hard to control ulcerative colitis with drugs and medicines. Sometimes this might not work. The person may then have to be admitted to hospital for more intensive treatment and care. Usually this works well. Once the inflammation is back under control the person can go home with a maintenance treatment programme.
Surgery
If the disease still does not respond to treatment, it is likely that surgery will be considered. The operation can remove the large bowel. This is called a colectomy. Sometimes only a part of the large bowel needs to be removed. Removing half of the large bowel is called a hemicolectomy. This type of surgery occurs mostly in people with Crohn’s disease and rarely in people with UC. Although surgery can seem a drastic step, it does cure the gut inflammation, as without a large bowel, there is no colitis.
In the past, a colectomy used to mean the fitting of a stoma bag. The bag is used to collect the waste that was disposed of via the large bowel before the surgery. But nowadays it is usually possible to remove the diseased bowel and rectum. Then construct a pouch of small bowel that acts very much like the rectum, giving no need for a stoma bag. It is important to note that this surgery is usually takes two to three operations. So, a stoma is likely to be needed for at least a short period of time. You can discuss the benefits and risks of surgery with your surgeon.
Diet
 Many people ask whether they should change their diet but there is no proven specific diet for ulcerative colitis. Healthy eating guidelines are advised. This consists of a wide variety of foods. Including fruit and vegetables, cereals, grains, protein-rich foods, nuts and seeds. Plus reducing foods in high fat, particularly animal fat, high sugar and processed meats. This can reduce the risk of bowel cancer.
Many people ask whether they should change their diet but there is no proven specific diet for ulcerative colitis. Healthy eating guidelines are advised. This consists of a wide variety of foods. Including fruit and vegetables, cereals, grains, protein-rich foods, nuts and seeds. Plus reducing foods in high fat, particularly animal fat, high sugar and processed meats. This can reduce the risk of bowel cancer.
Some people continue to have symptoms even though the inflammation has gone. These people have irritable bowel syndrome (IBS) symptoms as well as their controlled UC. People with IBS and ulcerative colitis may be able to manage symptoms by avoiding dietary triggers. Please ask your IBD team to refer you to a gastroenterology dietitian, if you feel that you are having symptoms related to food. Speaking to a dietitian is also helpful if you have unintentionally lost weight.
Smoking
 Research suggests ulcerative colitis is less common in people who smoke cigarettes. People who smoke and have ulcerative colitis have a milder condition and a slower disease course. It is not known what the reason is for this perceived benefit, as studies differ in what they find.
Research suggests ulcerative colitis is less common in people who smoke cigarettes. People who smoke and have ulcerative colitis have a milder condition and a slower disease course. It is not known what the reason is for this perceived benefit, as studies differ in what they find.
Smoking cigarettes has significant risk to health such as cancers, cardiac disease, strokes. So, it is still recommended that you stop. As there is a risk of having a flare after stopping, within the first 2 to 5 years, you should discuss stopping smoking with the IBD team. They may review your treatment to lower the risk of you having a flare-up.
Support
What to ask your doctor?
- Can I have the details for my specialist team, for example, my IBD nurse
contact details? - How often do I need to be seen in clinic?
- What should I do if I think I’m having a flare?
- What advice would you give if I’m planning a pregnancy?
- What advice would you give if I’m travelling abroad?
Where can I get more information?
The National Institute of Health and Care Excellence (NICE).
NICE make recommendations on a range of topics in health. They recommend the most effective ways to prevent and manage specific conditions. Plus how to improve health and manage medicines in different settings. You can find their guidelines on ulcerative colitis using the following link.
IBD UK is a partnership of 17 patient and professional organisations. These organisations are working together for everyone with IBD. They joined to develop standards that define what good care should look like for people with IBD.
IBDesis have created a fantastic video explaining IBD in South Asian languages.
Other support organisations
The UK leading organisation supporting people with Inflammatory Bowel Disease, including ulcerative colitis. This charity has comprehensive information on ulcerative colitis. This includes what benefits are available for people with ulcerative colitis. Plus, information on how to apply for personal independence payments (PIP).
CICRA (Crohn’s In Childhood Research Association)
There is a lot of research undertaken in ulcerative colitis. But many questions remain unanswered.
The James Lind Alliance (JLA) has carried out a Priority Setting Partnership (PSP) on inflammatory bowel disease. This includes ulcerative colitis. The PSP has identified 10 research priorities. People with UC and those who care for them decide what the priorities should be.
NICE has listed research questions in its guideline on ulcerative colitis. These guidelines are regularly updated. The research recommendations are likely to change to reflect new evidence.
Guts UK
Guts UK is proud to fund research into ulcerative colitis. This is alongside a large number of other digestive diseases.
 ABOUT US:
ABOUT US:
Guts UK’s vision is of a world where digestive diseases are better understood, better treated and where everyone who lives with one gets the support they need. We fund life-saving research into diseases of the gut, liver and pancreas.
Champion our cause; help us fight digestive diseases and change the lives of millions of people in the UK by supporting our work today.
DISCOVER OUR WORK:
Copyright © 2024 Guts UK. This leaflet was published by Guts UK charity in 2023 and will be reviewed in 2025. The leaflet was written by Guts UK and reviewed by experts in ulcerative colitis and has been subject to both lay and professional review. All content in this leaflet is for information only. The information in this leaflet is not a substitute for professional medical care by a qualified doctor or other healthcare professional. We currently use AI translation tools on our website, which may not always provide perfect translations. Please check for further explanation with your doctor if the information is unclear. ALWAYS check with your doctor if you have any concerns about your health, medical condition or treatment. The publishers are not responsible or liable, directly or indirectly, for any form of damages whatsoever resulting from the use (or misuse) of information contained or implied in this leaflet. Please contact Guts UK if you believe any information in this leaflet is in error.