Primary Sclerosing Cholangitis (PSC)
Download printable versionOverview
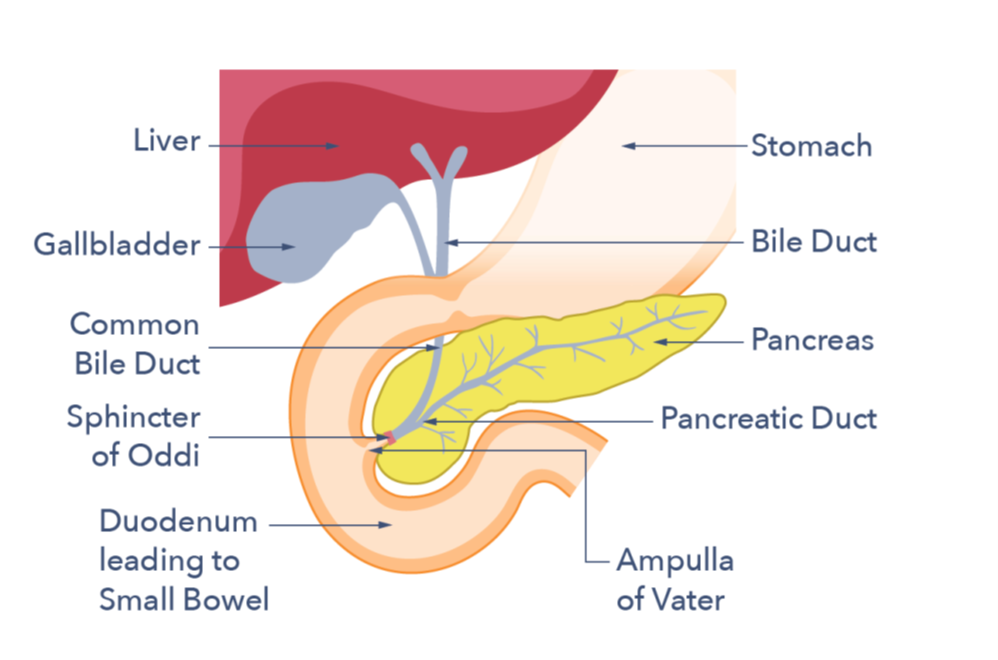
Primary Sclerosing Cholangitis (PSC) is a rare, immune related disease that affects bile ducts and liver. In PSC, bile cannot flow out of the liver properly due to narrowing’s (strictures) in the bile ducts. This can lead to a variety of complications, including bile duct infections, cirrhosis, bile duct cancer and/or liver failure although some patients have only mild symptoms.
Most people with PSC also develop inflammatory bowel disease (IBD) (Crohn’s disease and/or Ulcerative colitis) at some point in their lifetime. The inflammation is usually located to the large bowel (colitis). The colitis may be mild and asymptomatic and only diagnosed by examination of the bowel at colonoscopy but in other cases colitis in PSC can be aggressive and harder to treat compared with IBD that happens without PSC.
How common is Primary Sclerosing Cholangitis?
 PSC is a rare disease and affects approximately 7 individuals for every 100,000 people living in the UK. The disease is more common among those of Scandinavian heritage, and less so in people of Mediterranean extraction. The condition can affect people of any race. Also, any age (including children), with the highest rates of new diagnoses being made between the ages of 30-50 years. The disease is a little more common in men, who make up about 6 out of 10 people living with PSC, in the UK. Approximately 7 out of 10 people living with PSC will develop IBD at some point. In turn, between 5 to 20 out of 100 people with IBD develop sclerosing cholangitis over time.
PSC is a rare disease and affects approximately 7 individuals for every 100,000 people living in the UK. The disease is more common among those of Scandinavian heritage, and less so in people of Mediterranean extraction. The condition can affect people of any race. Also, any age (including children), with the highest rates of new diagnoses being made between the ages of 30-50 years. The disease is a little more common in men, who make up about 6 out of 10 people living with PSC, in the UK. Approximately 7 out of 10 people living with PSC will develop IBD at some point. In turn, between 5 to 20 out of 100 people with IBD develop sclerosing cholangitis over time.
Causes
What causes PSC?
The cause of PSC is not fully known, but research suggests that PSC is an autoimmune disease. Doctors and researchers suggest that certain genetic factors interact with unknown environmental or lifestyle triggers, to make a person more prone to develop the disease. The strong association with IBD suggests that changes in the gut bacteria are involved in disease development. PSC is not caused by alcohol.
Symptoms
How is PSC diagnosed?
There is no single diagnostic blood test for PSC. This means that your doctors need to piece together information from your medical history, blood tests, symptoms, colonoscopy and scans to make a diagnosis.
The gold standard tool for diagnosing Primary Sclerosing Cholangitis is an MRCP (magnetic resonance cholangiopancreatography). An MRCP is a type of MRI scan that looks closely at the bile ducts. It does not involve ionizing radiation.
Liver biopsies are not generally needed. But if the MRCP is normal and PSC is still a possibility, then a liver biopsy can be helpful in making the diagnosis.
What are the symptoms?
 PSC is highly variable between people and symptoms can come and go over time. For this reason, your medical history is important. This will establish whether your current symptoms are part of the regular pattern of your disease or if they represent a sudden deterioration.
PSC is highly variable between people and symptoms can come and go over time. For this reason, your medical history is important. This will establish whether your current symptoms are part of the regular pattern of your disease or if they represent a sudden deterioration.
In many people without symptoms, a PSC diagnosis is made by chance, after routine tests for IBD show abnormal liver blood results.
Other people may have the following symptoms:
- Feeling tired (fatigue)
- Having difficulties concentrating (‘brain fog’)
- Fever
- Feeling generally unwell
- Itching (particularly over the palms of the hands and/or soles of the feet)
- Yellowing of the skin or whites of the eyes (jaundice)
These symptoms trigger the above investigations to identify the cause.
Sometimes, particularly in children and young adults, the diagnosis of a different liver disease called autoimmune hepatitis (AIH) may be made first. Autoimmune hepatitis can then ‘evolve’ over time into PSC. Usually, people with an ‘AIH/PSC-overlap’ situation are identified when they do not get the full benefit from medicines used to treat autoimmune hepatitis. This situation is well-recognised among individuals who have IBD.
How can PSC affect you over time?

Unfortunately, there is no known medical treatment that slows down the rate of liver disease in people with PSC. However it is important to note that the course of PSC is very variable and some patients remain asymptomatic for many years.
The outcomes after liver transplantation are generally very good for PSC, but disease can develop again in up to 3 out of 10 people.
IBD activity can also ‘flare-up’ after transplantation in about 4 out of 10 of people, and colonoscopies must continue in people who have had a transplant for PSC.
Approximately 3 out of 20 people can also develop a cancer in their bowel or bile ducts. Bile duct cancers are most often diagnosed in the first two years after PSC diagnosis and less commonly picked up later in the disease course.
Treatment
What treatment is available for PSC?
 Liver transplantation is currently the only life-extending treatment for PSC, and no medicine has been shown to slow disease progression. However, there are several clinical trials underway to evaluate potential new treatments.
Liver transplantation is currently the only life-extending treatment for PSC, and no medicine has been shown to slow disease progression. However, there are several clinical trials underway to evaluate potential new treatments.
Ursodeoxycholic acid (UDCA) is sometimes prescribed for people with PSC. This medicine has been shown to improve liver blood tests in some people. However, there is no evidence that it slows the rate of liver disease, reduces cancer risk, or prevents a need for transplantation. It can be helpful to talk to your doctor about the risks and benefits of UDCA at low to moderate doses (i.e. between 17-22 milligrams of UDCA for every kg of body weight you are). Higher doses can lead to complications and should be avoided.
In some individuals, a procedure called an ERCP may be performed. This treatment is used to widen narrowings in the bile ducts. However, for most people with PSC several bile ducts are affected and this approach is not effective. It can be helpful to talk to your doctor about the risks and benefits of undergoing an ERCP.
Does PSC need monitoring?
PSC is a rare, complex condition, which increases the risk of some cancers.
Therefore, the team who are caring for you should include someone who has knowledge and experience of treating people with PSC. Your consultant will monitor your condition closely and help manage your symptoms using medical guidelines. Importantly, as an individual with PSC, it is your right to be offered the opportunity to participate in clinical trials of new and emerging medicines.
 Because PSC is rare and there are no currently available treatments, everybody who is diagnosed or suspected to have PSC should be offered discussion with a PSC specialist. Plus, access to clinical trials of new medicines, regular monitoring (as outlined above) and surveillance.
Because PSC is rare and there are no currently available treatments, everybody who is diagnosed or suspected to have PSC should be offered discussion with a PSC specialist. Plus, access to clinical trials of new medicines, regular monitoring (as outlined above) and surveillance.
Support
What to ask your doctor
- How can I contact you if I have concerns that I think relate to my PSC in office hours and out of office hours?
- What symptoms should I watch out for and what should I do if they occur?
- Is my PSC stable? If not, what are the next steps?
- How often will I need to see you for my routine care?
- What routine tests do I need now and how often?
- What do my test results mean?
- I am feeling worried/low. Where can I get help?
- Can I be referred for a PSC clinical trial in this hospital? Or if not available here, to the nearest PSC trial centre? (Some people switch hospitals temporarily for the duration of a clinical trial. This is so that their PSC care is managed at the hospital that is conducting the research. Or they have a ‘shared care’ agreement whereby they still see their regular hospital doctor, but also the researcher at the PSC trial centre.)
British Society of Gastroenterology/UK-PSC Guidelines for the Diagnosis & Management of PSC.
PSC SUPPORT
PSC Support is the UK charity supporting people diagnosed with PSC.
The PSC Support app helps people track their symptoms, find clinical trials and know what to expect from their care.
ACUTE CHOLANGITIS ALERT CARD
Acute cholangitis (sometimes called bacterial cholangitis) may occur in people with PSC, even in those with otherwise good liver function. The exact cause is not known but is thought to be the result of an infection of the bile ducts within the liver. Acute cholangitis in PSC can be difficult to recognise and signs and symptoms can vary from person to person. If you think you have acute cholangitis, seek urgent medical care. Left untreated, it can cause serious complications such as sepsis, jaundice and liver decompensation. You can order or download a free Alert Card. This has been developed by PSC Support and UK-PSC to help you and your doctor recognise the signs and make treatment decisions together.
Research
There is currently no known curative treatment, or treatment that is known to slow the progression of PSC. Research priorities are:
- The search for a curative treatment.
- Treatment which slows the progression of PSC.
- Treatment that alleviates the symptoms and psychological effects of PSC and improves quality of life.
- Treatment which improves outcomes after liver transplantation.
If you wish to search for any clinical trials that might be asking for people with PSC to be involved, you can read more on the PSC Support website.
 ABOUT US:
ABOUT US:
Guts UK’s vision is of a world where digestive diseases are better understood, better treated and where everyone who lives with one gets the support they need. We fund life-saving research into diseases of the gut, liver and pancreas.
Champion our cause; help us fight digestive diseases and change the lives of millions of people in the UK by supporting our work today.



