Karan’s story – Diverticulitis
"My life got turned on its head and I didn’t see it coming."
Tell us a little about yourself
“I’m Karan, I’m 51 years old and live in Lincolnshire with my husband, Steve, and our dogs. We have a 26-year-old daughter. I work at a local college in a pastoral care role, supporting students and ensuring their physical and emotional welfare.
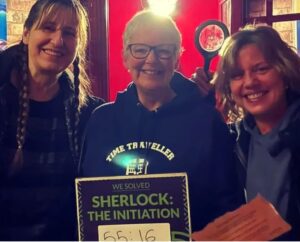
I love to spend time with my family and friends. My closest friends, Ellen and George (pictured below) have been there for me through thick and thin. I wouldn’t have coped without them.”
When did your diverticulitis symptoms begin? What were they?
“At the end of 2020, I started to experience period-like pain in my left-hand side. I had no other typical diverticulitis symptoms, like bowel problems. The pain didn’t go away and eventually my husband said, “This isn’t right, you need to go to the doctors.”
The GP thought it could be diverticulitis and prescribed me antibiotics, but the pain continued. My closest friend is a nurse and asked me how I’d been diagnosed without a colonoscopy and I said, “I didn’t know, I don’t know about medical stuff!””
What happened when you saw a doctor?
“I completed a FIT test (a faecal immunochemical test that can indicate bleeding in the lower digestive tract) and was referred to a gynaecologist. In November 2021, gynaecology immediately told me “This is a bowel problem”.
Just days later, things became much worse. My stomach was so bloated, and I felt so poorly. I vomited and went to bed. The next day, I got a GP appointment. Despite it being a short walk away, my husband had to drive me there. I couldn’t do it.
I couldn’t lie down to be examined or bear my stomach being touched and my blood pressure was very low. I was told to go to hospital.”
What happened at the hospital?
“After a four-hour wait, I was given a blood test and prescribed paracetamol. Eventually, I was put on an IV drip (a drip which delivers medication via the veins) and later that night, scans showed my bowel had perforated.
I had emergency surgery the following day and was told that I might need a colostomy (a surgical procedure that creates an opening in the large intestine or colon to divert the contents through the abdominal wall). 18cm of my bowel was removed and when I woke up in the high dependency unit after surgery, I had a stoma.”

How did it make you feel?
“It was a big shock. I couldn’t take in what had happened. I was on a lot of pain medication. Emotionally, the trauma really affected me.
I wore a clear stoma bag so that the hospital team could make sure everything was working properly. I fluctuated between thoughts of “Oh that’s quite cool to look at” to “What is that? How am I going to come to terms with it?” I worried if I could have a normal life again. I wondered if I would feel confident again. Would it change my relationship with my husband? What about work? Could I still go out with my friends and family?”
What about when you returned home from hospital?
“When I first went home and showered without my stoma bag on, my stoma started to move slightly as my bowel worked, which is normal, but I thought something was wrong. I was panicking and sobbing on the bathroom floor. I felt so frightened and wondered if anybody else had experienced this. I want to be the person who I needed then so I’m very open about my experiences.”
Do you still have your stoma now?
“I was told that a reversal (a surgical procedure that reattaches the bowel after a colostomy or ileostomy) could be an option. When I had my stoma, I thought, “I’ll get rid of it, I don’t want to be stuck with it forever” but after a while, I realised I didn’t have an issue with it.
However, I developed a large abdominal hernia that was causing me a lot of issues, and I questioned my decision. My bowel was now healthy, and I was told a reversal was possible. I felt fear. I’d been through so much trauma with the surgery and thought “I don’t want to go through that again. I can’t do it.”
In 2022 I was referred to counselling and in 2023, was put in contact with someone via my stoma nurse who’d had their stoma reversed. Although we’d never met, we chatted about all things poo and bowels. I felt so reassured that I’d be fine.
In March 2024, I had my stoma reversed and my hernia removed.
My surgical wounds needed dressing daily. However, I couldn’t get an appointment at my GP surgery. Fortunately, my friend Ellen, who is a nurse, visited me daily to do this. She’s my hero.”

Did you know about diverticulitis before your diagnosis?
“I didn’t know a thing about diverticulitis before my diagnosis. It wasn’t until I got discharged that I got an official diverticulitis diagnosis, which was shocking.”
Why are you sharing your story today?
“I want to be the person that I needed back then. I felt that nobody understood what I was going through and I had nobody to talk to about it. If I can help one person, that’s enough for me!
I know how important it is to talk. At work, I talk openly with my colleagues and the students I work with. I was scared I’d be judged but people shared their own stories with me too. One student, who was just 17 years old, asked me “I’ve got blood in my poo, should I go to the doctors?” When I asked her if she’d have spoken to anyone else about it had she not heard me speak about what I’d gone through, she said “no”.”

Tell us more about why you support Guts UK
“Ellen told me about Guts UK when I was in the first stages of diagnosis. She said, “Have a look, there’s loads of useful stuff on their website.” Your information is so user-friendly, relatable and understandable. It’s so reassuring.”
We’re getting to grips with guts!

Guts UK is the charity for the digestive system. Our guts have been underfunded, undervalued and misunderstood for decades. With your support, we can change that. Guts UK’s research life-changing leads to earlier diagnoses, kinder treatments and ultimately, a cure.
Help us by making a donation today.