Sharan’s story – Crohn’s Disease
Crohn’s has taught me to be my own advocate. Being honest doesn’t make you weak. It gives you control. Chronic illness doesn’t make you less capable. Anyone can become unwell. We all deserve understanding and support.
Tell us a little about yourself
“I’m Sharan. I’m Punjabi and live with my family in Berkshire. I am co-founder and Chief Digital Officer for Strategic Alliance for Intercultural Advocacy in GI (SAIA) and I trained as a Diagnostic Radiographer.”

When did your symptoms begin?
“In September 2001, I woke up one day with diarrhoea and abdominal pain. At first, I thought it was the heavy, spicy Indian food I had at my cousin’s wedding, but my symptoms didn’t stop.
My GP thought it was indigestion and prescribed medication, but nothing helped. By December, I started vomiting. I had an ultrasound (a medical imaging technique which uses sound waves to create images of inside the body), but nothing showed up. I vomited in class. It was humiliating and traumatising and I didn’t go back to school for the rest of the year. My parents watched me lose weight and struggle, but no one could tell us why.”
Talk us through your journey to diagnosis
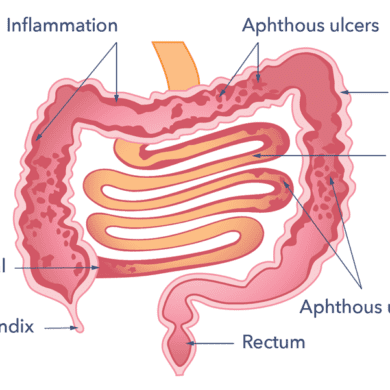
“By January 2002, I was losing more weight and vomiting after every meal. I was referred to a paediatric gastroenterologist who mentioned inflammatory bowel disease (IBD). He took bloods and prescribed me codeine for the pain, but it made me drowsy all the time.
By February, I became too weak to eat or drink, and I went to the paediatric day unit for treatment. They gave me fluids via my veins then transferred me to another hospital. After blood transfusions and a colonoscopy (a thin tube with a small camera on the end inserted via the back passage), I was diagnosed with Crohn’s disease.
It was a relief to finally have an answer but also terrifying. It was confusing for my parents as English isn’t their first language. Trying to translate what the doctors were saying was so hard. When I was told there is no cure. It hit me this is lifelong.”
What treatment have you received?
“I was started on enteral nutrition through a nasogastric tube (a soft tube which goes up the nose and into the small bowel). I felt embarrassed going to school with it, so I was homeschooled for a while.
After eight weeks, I tried food again, but my symptoms returned. I was prescribed prednisolone (a steroid medication to suppress inflammation), which helped at first, but the symptoms came back when the dose was reduced. About a year later, I had surgery to remove part of my bowel (a right hemicolectomy) and was prescribed azathioprine (an immunosuppressant medication to reduce inflammation over a longer period).

Moving to adult care was difficult. I often felt dismissed. University stress triggered flare-ups, and steroids became the default treatment. It wasn’t until I saw a new consultant that things started to change. He treated me as a person. He applied for me to start infliximab (a biologic medication), which wasn’t approved until after multiple hospital stays. It allowed me to finish university and start living again.
Later, I switched to adalimumab (a biologic medication), which I injected weekly, but in 201,3 I developed a stricture (a narrowing of the bowel), and a dilatation didn’t relieve it. In 2014, I needed emergency surgery and woke up with an ileostomy (part of the intestine is diverted to the surface of the tummy to create an opening).”

How did you adjust to life with an ileostomy?
“It took me approximately six months to come to terms with it. Over time, my energy returned, my pain eased, and I could eat without fear. I joined a local netball team, went back to swimming, and slowly regained confidence.
In 2016, my consultant suggested a reversal. Part of me didn’t want to go through another big surgery, but culturally, there was a lot of pressure. In South Asian culture, illness isn’t something we talk about openly. I worried about how to explain my ostomy to a future partner and their family.

I had the reversal, but soon I started flaring again. It was frustrating because I had been doing well with my ileostomy. I started seeing blood in my poo, and I knew something wasn’t right.
In 2019, a capsule endoscopy (where you swallow a small capsule with a camera to examine the digestive tract) showed active disease, and I began Ustekinumab (a biologic medication). It stopped the bleeding, though I have symptoms and occasional flare-ups now.”
Why do you feel it’s vital to be open about your digestive condition?
“Crohn’s is a real condition. It doesn’t define you, but it becomes a big part of your life. I used to hide it at work because I didn’t want to seem unreliable. I wasn’t ready to have those conversations when I was younger.

Now, I’m open. I know how to ask for adjustments at work, and my employers have been understanding, letting me create a shift pattern that works. Being honest doesn’t make you weak. It gives you control. Chronic illness doesn’t make you less capable. Anyone can become unwell. We all deserve understanding and support.”
What has living with Crohn’s disease taught you?
“Crohn’s has taught me to be my own advocate. Do your research. Ask questions. And take notes. If you’re not happy with your care, it’s okay to change hospitals or consultants. I’ve learnt how important it is to have information that truly represents you.

Ask for an interpreter or ask for materials in your language. Being South Asian, most of the advice I was given didn’t fit my diet or culture. I stopped eating the food I loved because I thought I wasn’t allowed to. If I’d have had the information I needed earlier, I probably wouldn’t have rushed to go to university and force myself to do everything that was ‘expected’ of me. Not having the information or support sparked my passion to become part of starting SAIA. It’s so important that everyone has representation and feels supported.”
Is there anything you’d say to someone with a digestive condition like Crohn’s disease?
“If you’ve just been diagnosed, reach out to organisations like Guts UK and Crohn’s & Colitis UK for support and information. Find support groups, online or in-person, where you can talk to people who understand what you’re going through. Look after your mental health as well as your physical health. I wish I’d had that support when I was younger. You carry so much uncertainty with this condition, and it’s okay to ask for help to process that.”
Why are you sharing your story today?
“I want to raise awareness about Crohn’s disease and the need for cultural understanding in care. South Asian families don’t always talk openly about health, and that needs to change. I want people to know it’s possible to live a full, meaningful life with Crohn’s. I’ve faced setbacks, surgeries and hard days, but I’ve also learned to advocate for myself and embrace life again. If my story helps even one person feel seen, that means everything to me.”
Why do you want to support Guts UK charity?
“Guts UK make information accessible and relatable for all ages, sharing stories that make a difference. I wish I’d seen that as a teenager. You also create space for diverse voices, and that’s something I’m passionate about. Through SAIA, we’ve built a great relationship with Guts UK, and I’m proud of how we’ve worked together to make digestive health more inclusive.”
What we do

Guts UK is the only UK charity funding research into the digestive system from top to tail; the gut, liver and pancreas.
People are suffering. People are dying. All because of a lack of knowledge about our guts. Guts UK exists to change that.
With new knowledge, we will end the pain and suffering for the millions affected by digestive diseases. Please consider donating today. Your donation will help fund research leading to earlier diagnoses, kinder treatments and ultimately, a cure.