Creating ‘miniguts’ to develop new treatments for IBD
Dr Paloma Ordóñez-Morán has created 3D ‘miniguts’ to help develop new treatments for Inflammatory Bowel Disease (IBD).
The few treatments available for inflammatory bowel disease (IBD) like colitis or Crohn’s disease don’t work for everyone. To better understand the complexity of IBD, Dr Paloma Ordóñez-Morán has generated small 3D gut-like structures in the lab from patient biopsies. These ‘miniguts’ could one day help develop and test new treatments that improve the lives of adults and children.
Inflammatory bowel diseases (IBD), like Crohn’s disease or ulcerative colitis, affect more than half a million adults and children in the UK. The inflammation in the bowel causes symptoms like diarrhoea, bleeding, pain, and fatigue, which flare up and die down in a way that can feel relentless. And for one in three people, the few treatments available can’t control their symptoms.
“It’s hard for adults – it’s hard to imagine what it’s like for children,” says Dr Paloma Ordóñez-Morán, from the University of Nottingham’s School of Medicine. “If their treatment does not work, their symptoms can keep them from having a normal life.”

The lack of treatments for IBD is partly due to the poor success rate of clinical trials. Only 5% of IBD drugs that enter clinical trials eventually get approved as a treatment, Paloma estimates.
She believes this can be traced back to the methods scientists use in the lab to study IBD, called ‘models’ of IBD. These models might include gut cells grown in flat sheets in the lab over many years, or mice which have IBD-like symptoms.
But no model is perfect. If these models don’t imitate the disease closely enough, drugs that seem successful in the lab might not work when they’re given to real people.
This is a huge disappointment after such a large investment of time and money – and meanwhile, people with IBD are left waiting for better treatments.
Creating miniguts
Creating better models to study IBD is part of Dr Paloma Ordóñez-Morán’s mission. She’s particularly interested in epithelial stem cells: the special cells that replace the entire inner lining of the gut every five days, and play a key role in repairing tissue after damage.
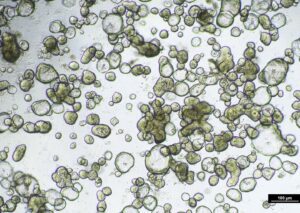
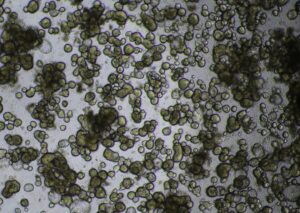
If they’re grown in the lab in just the right way, the epithelial stem cells can create small gut-like structures – a bumpy hollow ball which Paloma calls ‘miniguts’.
Guts UK awarded funding to Paloma to use these IBD miniguts to investigate how the stem cells respond to inflammation, and IBD treatments.
To create these miniguts, Paloma used samples collected during routine colonoscopies from the bowels of adults and children with IBD, as well as from healthy volunteers without IBD.
These samples were collected by the nurses and clinical team from Queen’s Medical Centre in Nottingham. “Their commitment and professionalism were invaluable in making this research happen,” Paloma says.
The IBD miniguts recreate some of the features of IBD as it occurs in people, such as scarring, which can cause narrowing of the bowel that may lead to life-threatening obstructions.
Another important finding of the project was that IBD miniguts respond to inflammation differently compared to ‘healthy’ miniguts grown from people without IBD. This suggests you can’t test new treatments on just anyone’s miniguts – you need to use IBD miniguts from people with IBD.
Testing new treatments
Paloma continues to improve the miniguts to make them an even better model of IBD. As well as helping to better understand how stem cells behave in IBD, her miniguts have received a lot of interest from pharmaceutical companies, which hope to use them to test new potential IBD drugs.
The miniguts could help researchers spot at an earlier stage which drugs have little chance of success. If those drugs can be discarded before they reach a clinical trial, the money and effort saved can be redirected towards other drugs that look more promising.
“Even if the miniguts model isn’t perfect, it’s better than before,” Paloma says. “There will be less time and money spent if you could test fewer drugs. Right now, only around 5% of drugs that reach clinical trials are successful. If we get that to 30%, or even 50%, that’s already a huge success.”
Eventually, Paloma hopes the miniguts can help deliver better treatments, quicker – and help more adults and children live without the burden of IBD.
Supporting research is the best way to go forward
Despite the number of people affected, inflammatory bowel diseases don’t receive a lot of research funding, compared to other diseases like cancer. But this means funding from charities like Guts UK is even more appreciated, and can have a bigger impact. “There’s a lot we can do with the new technology available,” says Paloma, “there are many things to be done that have not been done yet.”
Paloma’s miniguts could soon be helping to develop and test new treatments for IBD – something she says wouldn’t have happened without the funding from Guts UK’s supporters. “I don’t know how much I can thank them with words – it has been essential for the development of this project,” Paloma says. “I think that supporting research is the best way to go forward and improve the current situation.”



