Sue’s story – Diverticular disease
“The constant anxiety of not knowing when symptoms will flare up makes it an isolating illness. It affects every part of daily life from what I eat, where I go, and how I feel about myself.”
Tell us a little about yourself

“I’m Sue, and I live in Tameside. I retired last November after a long career working in housing, everything from homelessness support to being a housing officer in prisons for those who are released, which was rewarding but often stressful.
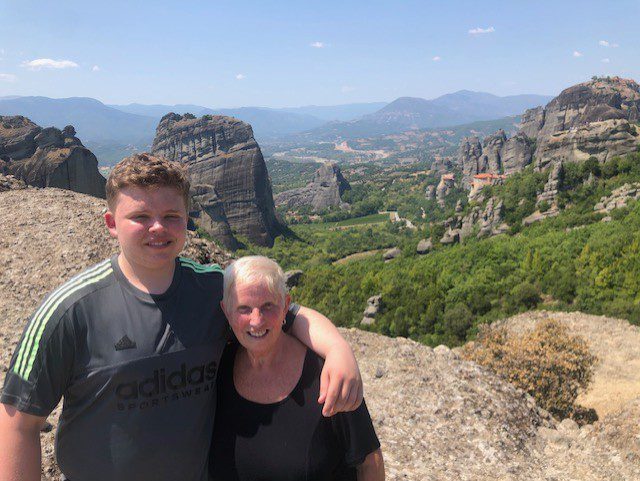
Family means a lot to me. I have two children, Matthew and Natalie, who are both in their forties, and a grandson, George, who’s now 15.
Now that I’m retired, I’m making the most of my time by travelling as much as I can. I’ve just come back from Devon to see a friend, and I’m going on a cruise with my grandson to explore the Greek islands.”
When did your symptoms begin, and what were they?
“My symptoms first started in my mid-to-late twenties. At the time, I was told it was Irritable Bowel Syndrome (IBS), as they didn’t do many investigations back then. I experienced painful stomach cramps and diarrhoea that made everyday life difficult. It wasn’t until my late thirties, after I became very unwell one night and ended up in hospital, that they carried out more tests and diagnosed me with diverticular disease. Despite the diagnosis, I was offered no real treatment or follow-ups.
How has diverticular disease affected you in more recent years?
“For many years, I just lived with the ongoing symptoms as best I could. But things changed a few years ago when I developed sepsis after a severe flare-up. I was admitted to hospital for several days, and initially I was told I couldn’t go on a holiday I had planned. It was very frightening. Over the following year, I had two more serious flare-ups that landed me back in hospital. Each time, doctors spoke to me about the possibility of needing a stoma, though in the end, I was sent away with antibiotics.
Although I haven’t had another major infection for over a year, those hospital admissions left a lasting mark. Living with diverticular disease feels like having a shadow hanging over me. You never know when the next flare might hit, or whether this time it will mean surgery and a stoma (an opening on the abdominal surface to divert the flow of poo into a bag). That constant uncertainty and anxiety can be as hard to cope with as the physical symptoms.”
What are the day-to-day challenges of living with diverticular disease?
“The biggest challenge is the unpredictability. I can wake up feeling fine, and then suddenly be doubled over with pain and needing to rush to the toilet again. It makes everyday life very difficult to plan. I always need to know where the nearest toilet is, and I get anxious about being in situations where I can’t get out quickly.
Food is another challenge, and I have felt restricted when it comes to understanding which foods I can still enjoy. I can’t eat spicy or fried foods and have very few sweet treats. If I’ve got to go on a journey, I’ll often avoid eating whilst travelling just so I can get through it. That means I’m often low on energy, but it feels like the safer option. Even holidays, which should be enjoyable, take a lot of careful planning around food, toilets, and timing.
Note: Everyone’s experience with digestive conditions is different. Guts UK does not recommend restricting or removing food groups without medical guidance. If you face dietary challenges, please ask your GP for a referral to a dietitian for ongoing support.
There’s also the emotional side. It’s embarrassing to talk about bowel problems, and the accidents I’ve had over the years have left me feeling humiliated at times.”
Tell us about your involvement in the diverticular disease Priority Setting Partnership (PSP)?

Note: The last stage of the diverticular disease PSP took place In February 2025, where a group of patients, family members, clinicians and researchers came together to decide the top ten research priorities for diverticular disease.
“I got involved with the PSP a couple of years ago after joining a diverticular disease support group online. I decided to get involved because I’ve lived with this condition for so many years and I really want to see more awareness, research, and hopefully better treatment options for people in the future.
For me, one of the most valuable parts was just being in a room with people who truly got it. Both professionals who genuinely cared and other patients who understood exactly what living with this disease is like.”
Tell us about your experience with having a colonoscopy and how that linked in with your involvement with the PSP?
Note: A colonoscopy is a thin tube with a small camera on the end inserted via the back passage.
“My experience was traumatic. I found it unbearably painful and had to ask the team to stop partway through, which left me in tears after going through all the exhausting preparation beforehand. Later I learned that, because I’d had a hysterectomy, scar tissue may have made the procedure more difficult, and I probably should have been assessed differently from the start.
When I later had a CT colonoscopy (a non-invasive virtual coloscopy that uses a CT machine and X-ray to provide imaging), it was far easier and much less painful. Going into the PSP, I felt strongly that research should look at better, less invasive ways of diagnosing and monitoring diverticular disease.
During the discussions, I came to understand why professionals ranked it lower, because alternatives like CT colonography already exist and my painful experience should never have happened in the first place. Having the chance to share my experience and be listened to by surgeons, GPs and researchers was empowering and helped me feel that our lived experiences really mattered.”
Why did you want to share your story with Guts UK today?

“Diverticular disease is such a painful, isolating condition, and I don’t think people realise just how much it affects everyday life. It’s not something people like to talk about, but that makes it even lonelier when you’re going through it.
I hope to raise awareness so that others understand what it is really like to live with this condition. I also want people who’ve just been diagnosed to know they’re not on their own — there’s a whole community out there, and charities like Guts UK are working hard to push for research and better treatments.”
About Guts UK

Guts UK is the national charity for the digestive system and the only UK charity funding research into the whole digestive system.
People are suffering. People are dying. All because of a lack of knowledge about our guts. Guts UK exists to change that.
With new knowledge, we will end the pain and suffering for the millions affected by digestive diseases. Please consider donating today. Your donation will help fund research leading to earlier diagnoses, kinder treatments and ultimately, a cure.