Frankie’s Story – Irritable Bowel Syndrome (IBS)
"I remember thinking, “No one wants to be out at a club at university and needing to rush to the toilet.”" Frankie shares her Irritable Bowel Syndrome (IBS) experiences, keen to encourage others to not suffer in silence.
Tell us a little about yourself
“I’m Frankie and I’m 22. I’m a Fundraising Administrator here at Guts UK. I live in Essex at home with my parents, siblings and our puppy. In my spare time, I love reading, crocheting and knitting.”

When did your Irritable Bowel Syndrome (IBS) symptoms begin, and what were they?
“My IBS symptoms are excessive wind, bloating and nausea. This tends to be accompanied with abdominal pain, and I also experience extreme urgency with diarrhoea.
It’s hard to pinpoint when my IBS symptoms began, as I had symptoms since primary school. Doctors thought I had a gluten intolerance. Fast forward to 16 years old, things got worse. I didn’t enjoy school which caused me a lot of stress, and I ended up taking days off school with diarrhoea. During the Covid-19 pandemic, I tried going lactose-free, which just made things worse when I reintroduced it. I just ignored things for a while and tried to get on with it.”
Note on identifying trigger foods: It’s important to speak to a dietitian before trying exclusion diets.
“When I was 18 and studying at university, I knew that what I was experiencing wasn’t normal. I spoke to my mum, who is a nurse, and she prompted me to get a GP appointment. The GP ran tests, and my calprotectin (inflammation markers in the gut) was raised. I had the test repeated, and it showed slightly raised markers. My GP said to treat it as IBS-D (IBS with diarrhoea), so I tried healthy eating habits and dietary management. Things still weren’t great, but I didn’t feel confident to go back, so I carried on as best as I could. I remember thinking, “No one wants to be out at a club at university and needing to rush to the toilet.”
Note for diagnosis of IBS: The GP will want to rule out other conditions but will probably make a diagnosis based on the described symptoms. After ruling out other conditions with a few simple tests, doctors can be confident the diagnosis is IBS. This then allows the person to try treatments to reduce the burden of symptoms.

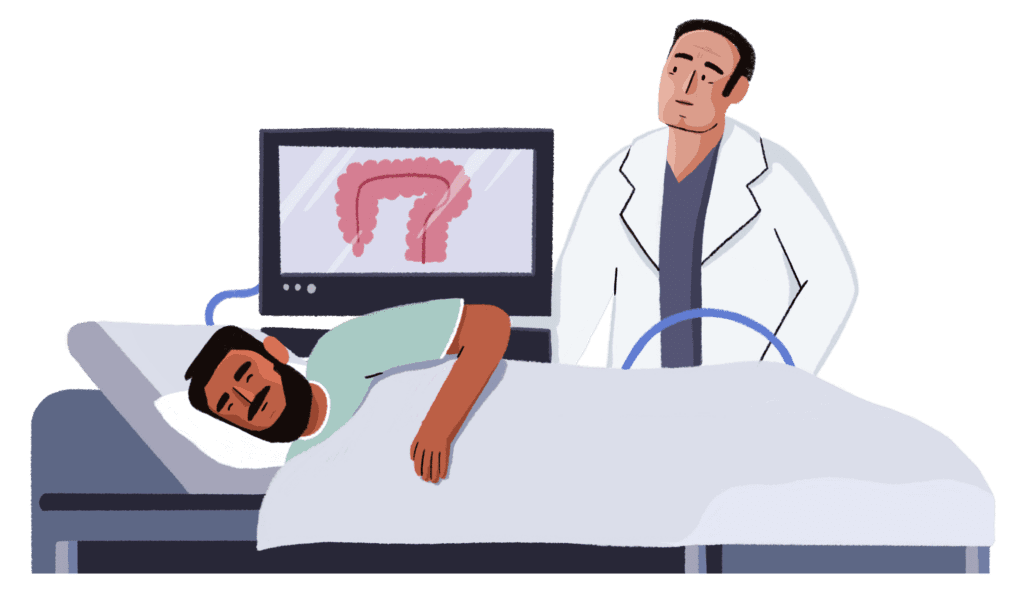
Tell us about your colonoscopy experience
“I finished university and found my job at Guts UK. Things still weren’t right. At the start of 2025, I reached back out to my GP. I had further tests, and my calprotectin levels came back very high (which can be a sign of Crohn’s disease or ulcerative colitis) and were slightly elevated with further testing.
This time, I pushed to see a gastroenterologist (a healthcare professional who specialises in the diagnosis and treatment of conditions affecting the digestive system) and in July, I saw a Gastroenterology Triage Nurse. A colonoscopy (a thin tube with a small camera on the end inserted via the back passage) was arranged. The preparation for the colonoscopy was the hardest part for me. I slept on the bathroom floor the night before so I could be close to a toilet and felt awful.
The day of my appointment arrived, and I felt anxious. I felt out of place as the waiting room was full of people much older than me. One of the nurses said to me, “Your birthday is in the 2000s? We don’t see that often!” which made me feel even more anxious. It was difficult for my cannula to be put in place for my colonoscopy because I was cold and very dehydrated from the bowel preparation. However, everything went ahead, and I was sedated. I was awake for the procedure, but I thankfully felt unbothered by what was going on. It was interesting seeing my gut on the screens in theatre and how it reacted to different things. A polyp was taken, which they dyed blue to help them remove it, and I asked why my insides were going blue! They told me that no signs of inflammatory bowel disease (IBD) had been found.”
How did the test results make you feel?
“I was relieved, but I panicked about the polyp. You hear that word, and it’s very scary. I was sent home with a form with my bowel images on, including my blue-dyed polyp!
I got my results on the NHS app, which said the polyp was ‘significant’, with no further explanation, which heightened my anxiety. Months later, I was then told I have IBS again, and I’m still waiting on a GP appointment to decide the next plan of action.”

Can you tell us about how your IBS diagnosis has impacted you emotionally?
“It was a relief, but at the same time, I felt overwhelmed, as when it comes to IBS, it isn’t fully understood, and a diagnosis of IBS is often given where other conditions have been tested for and eliminated. Sadly, in the past, I felt disbelieved and shrugged off by doctors after I kept a journal of my symptoms and reached out for help. It’s exhausting to stand up for yourself repeatedly. That’s on top of the exhaustion you’re already feeling. The continuity of care is also not there.”

What do you wish people understood about IBS?
“IBS is a digestive condition which is well-known and quite normalised, which is great, but I feel like a lot of people just think you can just get on with your life as normal. They don’t see my different triggers or how I can go from being fine to feeling the opposite from one week to the next. There’s so much misinformation out there as well, which is terrifying, and it scares me to know that if I didn’t work at Guts UK, I’d probably believe it.
It wasn’t until after my colonoscopy that I found out about the different tests and conditions my family have had experience with, especially my grandparents. Their generation doesn’t talk about it and often suffers in silence. But because I’ve been more open about things, I think it’s helped them to be more open too.”

Why are you sharing your story?
“Encouraging conversations means more people talk about the things that are impacting them, and they don’t suffer in silence. Through speaking to fundraisers at Guts UK, I hear too many stories of people not feeling that they can reach out to get help, or feeling ignored when they do, and that needs to change. Digestive symptoms and conditions can happen to anyone at any age. It’s important to normalise this, especially to reduce the embarrassment and stigma that too often surrounds our guts.”
About Guts UK
Guts UK is the national charity for the digestive system and the only UK charity funding research into the whole digestive system.
We provide information and support for people affected by digestive conditions like irritable bowel syndrome, including a dedicated Helpline.
With your support, we can be there for people like Frankie when they need us most.