Diverticular Disease
Download printable versionOverview
Diverticular disease is a common condition. It affects around 1 in 3 people, and this increases to 1 in 2 people as they get older. It affects both men and women.
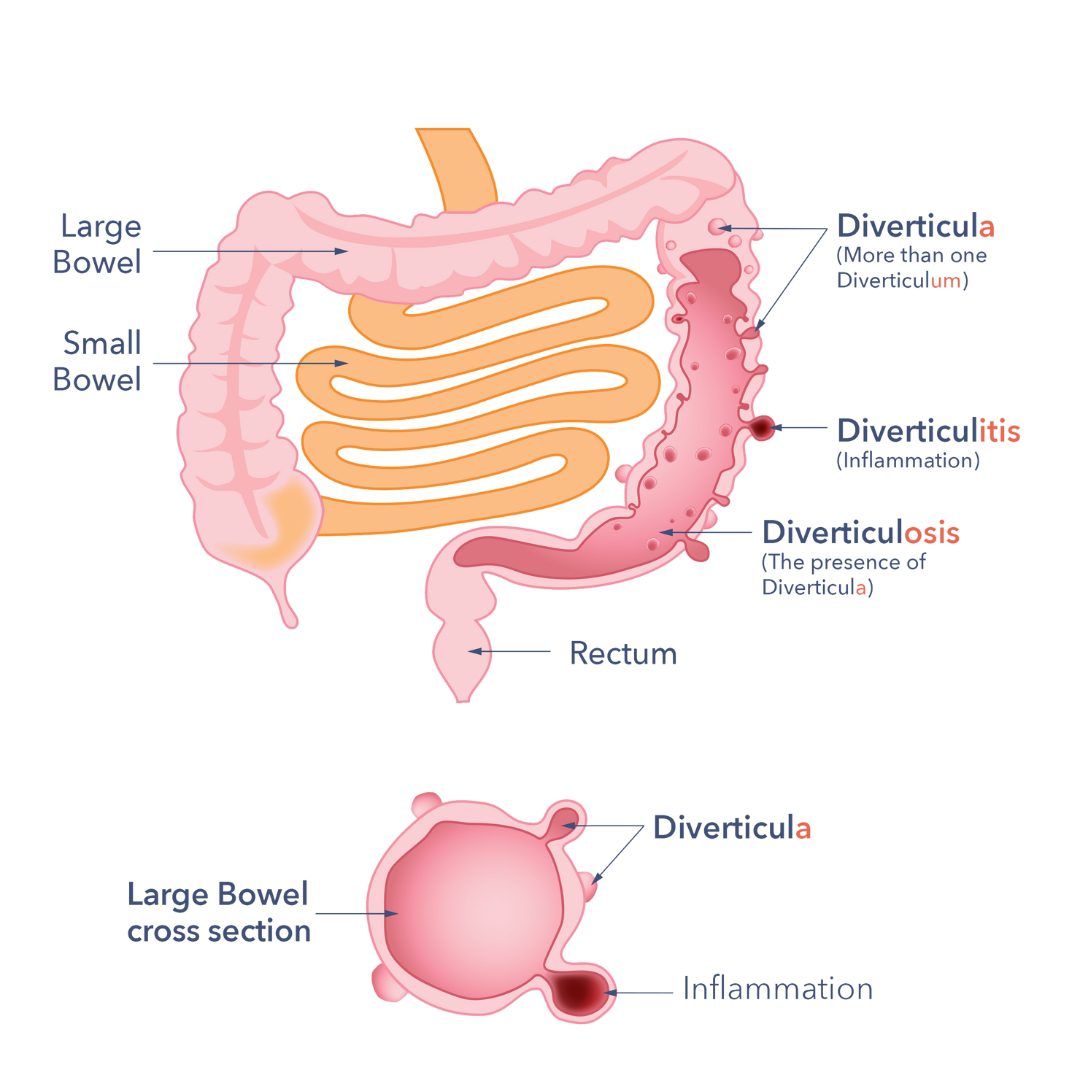
It happens when small pouches form in the wall of the large bowel. These pouches are called diverticula.
Understanding the different terms
- Diverticulum: this is a small pouch that sticks out from the wall of your large bowel.
- Diverticula: this means more than one diverticulum. They are most often found in the lower left part of the bowel.
- Diverticulosis: this means you have diverticula in your bowel. Most people with diverticulosis don’t have any symptoms and won’t need treatment. Many people don’t know they have it until they have a test for something else.
- Diverticular disease: this means you have diverticula. You might also feel belly pain or notice changes in your bowel habits, like constipation or diarrhoea.
- Diverticulitis: this happens when one or more diverticular pouches get inflamed or infected. This can cause increasing pain and other symptoms.
Causes
Diverticula form when the wall of the bowel becomes weak in places, which can happen as we get older. Pressure inside the bowel can then push the lining outwards, forming pouches.
Doctors still aren’t exactly sure why diverticula form in the bowel. But we do know some things that make it more likely.
Age is the biggest risk factor
Diverticula are more common as people get older and your chances of developing them increases after the age of 40. The number of people affected by diverticula is increasing to 1 in 2 as the population gets older. More young people under 45 are now being diagnosed, but this is still uncommon.

Other things that may increase the risk
Some lifestyle factors can raise the risk of symptoms or complications. These include:
- Having a higher than healthy body weight.
- Not being physically active.
- Smoking, which is linked to a higher risk of needing hospital care.
What about fibre and constipation?
- Some studies suggest that eating more fibre, especially from vegetables, may lower the risk of diverticula. However, other studies find no clear link.
- It is also not proven that constipation causes diverticula.
Genetic conditions (rare causes)
Some rare family conditions can weaken the bowel wall. This makes diverticula more likely. These include:
- Ehlers-Danlos syndrome
- Williams syndrome
- Polycystic kidney disease
- Marfan syndrome
- Coffin-Lowry syndrome
These conditions can affect the tissue in the bowel, making it weaker and more likely to develop diverticula.
Symptoms
Most people with diverticular disease do not have any symptoms. Even fewer people will go on to have complications.
When symptoms do happen, they may include:
- Pain or cramping in your lower belly (usually on the left side).
- A feeling of bloating or swelling in your belly (from gas).
- Changes in your bowel habits. These can include diarrhoea, constipation, or switching between both.
- Mucus or blood in your poo.
Everyone’s symptoms can be a bit different. The pain may come and go and is often worse after eating. It may feel better after you’ve been to the toilet for a poo or passed wind.
In people of South Asian background, the pain is sometimes on the right side instead of the left.
Important: Don’t ignore new symptoms. The symptoms of diverticular disease can look like those of other conditions, such as:
So it’s important not to assume that all belly problems are caused by diverticular disease.
See your GP if you:
- Notice any new or different symptoms.
- Have blood in your poo.
- Are being sick (vomiting), feel very bloated, have cramping pain and can’t poo or pass wind. This may be a sign of a blockage or complication, and you should get urgent medical help.
Complications
Very few people have complications severe enough to require hospital admission. Also, very few people die from this common disease. However, complications can occur in some cases. These include:
Inflammation (Diverticulitis)
This is the most common complication. The current theory is that the inflammation and/or infection occurs because of an overgrowth of bacteria in the diverticula. It occurs in up to a quarter of people with the condition. In people over 50, acute diverticulitis is more common in females. In those under 50 years of age, it occurs more commonly in males. More people are being diagnosed, especially people under 45.
Symptoms of diverticulitis:
- Worsening belly pain.
- High temperature.
- Feeling sick and being sick.
If these symptoms occur, you should seek medical help immediately. Complicated diverticulitis requiring hospitalisation is normally treated with antibiotics (germ-killing medicine) and fluids.
In severe cases, infection can cause complications, such as:
- A collection of pus (abscess).
- An obstruction (blockage of the bowel).
- Or a perforation (developing a hole in the bowel).
If these complications arise, an operation may be needed. It would remove part of the large bowel. Or a needle may be needed to drain a collection of pus.
Blockage of the gut
Thickening (fibrosis) can occur around areas of diverticulum that have experienced multiple episodes of inflammation. This may lead to narrowing of the large bowel, which can cause a blockage. These narrowings are also referred to as strictures. If diagnosed, surgery is usually needed.
Perforation
Sometimes, an inflamed pouch (diverticulum) can burst. It causes a hole in the bowel wall called a perforation. A perforation can cause an abscess or, more rarely, peritonitis. Peritonitis is a serious condition with widespread abdominal inflammation and infection that nearly always requires emergency surgery to treat.
Bleeding
A blood vessel in a diverticulum can burst. This can cause bleeding in the large bowel. 1 in 3 people with bleeding can have a severe episode. It may require a hospital admission.
Fistulas
Rarely, abnormal connections can form between diverticula and other organs. Organs affected include the bladder or vagina. These connections are called fistulas. Symptoms include:
- Poo in urine.
- Foul-smelling vaginal discharge.
If fistulas are diagnosed, surgery is usually necessary. So, see a doctor if you have these symptoms.
Is there a risk of cancer?
There is no evidence that having diverticular disease, whether you have symptoms or not, increases your risk of bowel cancer.
However, it’s still important to be aware of any new or changing symptoms. That’s because:
- Bowel cancer is common in the general population, especially as people get older.
- Some symptoms of diverticular disease can be like those of bowel cancer.
Always speak to your GP if your symptoms change, get worse, or you notice something new. Especially blood in your poo, unexplained weight loss, or ongoing changes in your bowel habits. These symptoms may not be caused by cancer, but it’s important to get them checked early.
Diagnosis
Doctors diagnose diverticular disease by looking inside your bowel or by doing a scan. These tests also help rule out other conditions that could be causing your symptoms.
Colonoscopy or sigmoidoscopy
A thin, flexible tube with a small camera on the end is passed into your bowel through your bottom. This allows the doctor or nurse to see the inside of your large bowel.
A colonoscopy looks at the whole bowel, while a sigmoidoscopy looks at just the left side of the bowel.
It is important that the bowel is empty so that they can see the bowel wall. You will be given a medicine to take at home to make you poo. This medicine will give you loose watery diarrhoea, so you will need to make sure you stay close to a toilet.
CT scan (plain CT)
This is a type of scan that takes pictures of the inside of your belly. It can show signs of diverticular disease and can also help find complications, such as an abscess (a pocket of infection).
CT colonography
This is a type of CT scan that looks more closely at the bowel. It’s a non-invasive test and doesn’t involve putting a camera inside the bowel. A thin tube may be inserted into the rectum to inflate the colon with air, making it easier to see.
Like a colonoscopy, you’ll need to empty your bowels before the scan using a special medicine called a laxative.

Treatment
Even with research on this condition, it’s still unclear why some people develop complications like infections. Many people can control their symptoms by changing their diet and lifestyle.
The exact cause of flare-ups isn’t fully clear. However, a healthy lifestyle may lower the risk of complications.
Diet and lifestyle
Eating well is one of the most important ways to manage diverticular disease.
What to eat:
- Follow a healthy, balanced diet.
- Include wholegrains, fruits and vegetables every day.
- Try to have a fibre-rich starchy food (like wholemeal bread, pasta, brown rice or potatoes with skin) with each meal.
- Aim for at least 5 portions of fruit and vegetables per day.
- 1 portion = about 80g or a handful.
- Smoothies (150ml) count as only one portion per day, no matter how much you drink, because they contain less fibre.
Drink enough fluids:
- Try to drink at least 2 litres (about 8 to 10 cups) of water or other non-caffeinated drinks each day.
- This helps fibre move through your bowel and can prevent constipation.
If you’re not used to eating much fibre:
- Increase fibre slowly to avoid bloating or wind.
- It might take a few weeks for your bowel habits to improve.
Do I need to avoid certain foods?
You don’t need to avoid seeds, nuts, popcorn, or fruit skins. These foods do not increase the risk of complications, even if you have diverticular disease:
| Starchy foods | Wholemeal, brown or granary bread. Oat or rye bread. Wholegrain crackers, wholegrain rice and wholegrain pasta. Wholegrain breakfast cereals, wheat bisks and non-wholewheat options such as oats, museli and gluten free wholegrain cereals. Chapatti or naan bread made with wholegrain flour. |
| Fruit | All varieties are suitable including fresh, frozen, dried and canned. |
| Vegetables | All varieties are suitable including fresh, frozen, dried and canned. Vegetable soup. |
| Protein containing foods | Chickpeas, lentils, peas and beans, dhal. Nuts and seeds. |
| Desserts and other snacks | Puddings containing dried fruit, oat-based crumble toppings, biscuits containing wholegrain flour, nuts, dried fruit and seeds, flapjack, muesli bars and fruit bars based on dates. Chocolate containing nuts and dried fruit, root vegetable crisps. |
| Drinks | Smoothies and milk shakes containing the whole fruit. (150ml portion size. One portion per day counts as one of your 5 fruit and/or vegetables per day). |
If you also have irritable bowel syndrome (IBS), eating more wheat bran can make your symptoms worse. If your symptoms don’t improve, try increasing your bran fibre intake using non-wheat bran options, like oat or rice bran. These are usually easier for people with IBS to digest.
If you change what you eat, it’s important to make sure your diet stays balanced and provides all the nutrients your body needs.
Try to limit red and processed meat to no more than 70 grams a day. If you eat red meat, unprocessed options are a healthier choice. Red meat includes beef, lamb, pork, veal, venison, goat and mutton. Processed meat includes sausages, bacon, ham, salami, corned beef, tinned meat, sliced luncheon meats, and pâté.
Information about healthy eating, fibre and IBS
Visit our online information:
Or contact us:
- E-mail: info@gutscharity.org.uk
- Call: 020 7486 0341
When to ask for more help
You can ask your GP or consultant to refer you to an NHS dietitian if:
- You have another medical condition that affects your diet.
- You’re unsure about what foods you should be eating.
- You still have symptoms such as gas, bloating or diarrhoea.
See your GP if your symptoms change.
Other ways to look after your health
- You should take regular exercise.
- If you’re overweight, try to lose some weight.
- Stop smoking. It’s one of the best things you can do for your health. Stopping smoking can be hard, but getting support makes it easier. Your GP can refer you to a local stop smoking service.
What about probiotics?
Some people try probiotics (good bacteria) to help with diverticular disease. But at the moment, there’s not enough good evidence to say they work. So, we don’t recommend using probiotics for this condition now.
Medicines
If you have constipation or diarrhoea, speak to your pharmacist or GP. A bulk-forming laxative might help. These work by absorbing water in your bowel, which can help manage both constipation and diarrhoea.
If you have pain caused by diverticular disease, your doctor might suggest trying an antispasmodic medicine such as Mebeverine hydrochloride.
Avoid using painkillers like codeine or other opioid-based medicines, as they can make constipation and pain worse. You can read more about this in our information on opioid-induced bowel dysfunction.
Other medicines that may cause problems include:
- Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen.
- Nicorandil, a medicine sometimes used for angina.
Both opioids and NSAIDs have been linked to serious complications such as fistulas and bowel perforation.
Important: Do not stop taking any prescribed medicines without talking to your doctor. They may be able to offer a safer alternative.
If you have diverticulitis (inflammation)
Your doctor may suggest a ‘watch and wait’ approach, especially if symptoms are mild. In some cases, antibiotics may be used, for example, if you are unwell, have a weakened immune system, or have other health conditions.
Contact your GP straight away if your symptoms get worse. See the section on diverticulitis (inflammation) for more about symptoms.
When is surgery needed?
Surgery for diverticular disease is not usually needed. But it may be offered after a serious episode of inflammation, for example, if:
- An abscess (a collection of pus) forms around the bowel.
- An infection spreads into the abdomen from a perforated (torn) pouch.
In most cases, the operation involves removing the part of the bowel that has the infected or damaged pouches.
Sometimes, the surgeon will need to bring the healthy end of the bowel out through the skin as a stoma. This allows waste to leave your body into a bag attached to your tummy.
In many cases, this stoma is temporary and can be reversed later. This means the bowel can be rejoined if the inflammation has settled and the area has healed well.
Bleeding
Sometimes, diverticular disease can cause bleeding from the bowel. In rare cases, this bleeding can be severe. If this happens, you may need an emergency blood transfusion. In most people (8 out of 10), the bleeding stops on its own without any treatment.
If the bleeding doesn’t stop, your doctor may arrange a special type of CT scan to find out where the bleeding is coming from. In many cases, this can also be used to stop the bleeding.
Other treatments using an endoscope (a thin, flexible tube with a camera) may also help. Your doctor or nurse will explain which treatment is best for you.
Myths
You might come across outdated or incorrect advice online about diverticular disease and what foods to avoid.
In the past, people were told not to eat certain high-fibre foods like:
- Seeds
- Nuts
- Popcorn
- Fruit skins
It was once believed these foods could get stuck in the diverticula (small pouches in the bowel) and cause problems. But this is no longer thought to be true.
These foods do not increase the risk of diverticulitis or bleeding. In fact, research shows:
- Men who ate nuts and popcorn had a lower risk of diverticulitis and bleeding.
- Women who eat more fibre were less likely to develop diverticulitis.
So, unless your doctor or dietitian tells you otherwise, these foods can be enjoyed as part of a healthy, balanced diet.
Some people are told to eat less fibre during a flare-up of diverticulitis (inflammation or infection of the diverticula). But recent reviews show that:
- There’s no good evidence that a low-fibre or low-residue diet helps people recover faster, have fewer symptoms, or avoid future episodes.
- A normal, balanced diet may be just as effective for people with uncomplicated diverticulitis.
If your diverticulitis becomes more serious — for example, if you develop a fistula, abscess, bowel blockage, perforation, or if you’ve had surgery — your doctor or dietitian may give you different advice based on your specific needs.
Support
What to ask your doctor
It’s okay to have questions about your condition and treatment. Here are some helpful questions you might want to ask your doctor:
- Has my colonoscopy or CT scan ruled out any other conditions?
- Are there any concerns about my large bowel?
- Can you refer me to a dietitian to help me manage my diet?
- What kind of follow-up or monitoring will I have?
- When would antibiotics be used to treat my diverticulitis?
- When should I get back in touch or seek more help?
Where can I get more information about treatment?
You can find reliable, evidence-based information from the National Institute for Health and Care Excellence (NICE). They provide clear, evidence-based guidance on a wide range of health, public health, and social care topics.
NICE provides guidance on:
- How to prevent and manage different health conditions
- The most effective treatments and medicines
- Ways to improve health and care in various settings
- Their recommendations are based on the best available research and are used by the NHS to help guide treatment and care. You can visit the NICE website to learn more and find their guidelines here.
References are available on request if you contact Guts UK.
Watch our diverticular disease webinar on demand
Discover more about diverticular disease and hear from healthcare professionals and people with lived experience of the condition:
Research
Guts UK has funded a ‘Priority Setting Partnership’ (PSP) to help identify the most important areas for research into the condition. Healthcare professionals, patients and their families have developed the top 10 priorities for future research. Read more here.
It is important that research into the causes and treatments for diverticular disease continues. Guts UK is the only UK charity funding research into the digestive system from top to tail. We’re proud to provide patient information about diverticular disease and are here to help. Please contact us with any questions that you may have.

Discover more:
Copyright © 2026 Guts UK. This leaflet was published by Guts UK in December 2025 and will be reviewed in December 2027. The leaflet was written by Guts UK and reviewed by experts in diverticular disease and has been subject to both lay and professional review. All content in this leaflet is for information only. The information in this leaflet is not a substitute for professional medical care by a qualified doctor or other healthcare professional. We currently use AI translation tools on our website, which may not always provide perfect translations. Please check for further explanation with your doctor if the information is unclear. ALWAYS check with your doctor if you have any concerns about your health, medical condition or treatment. The publishers are not responsible or liable, directly or indirectly, for any form of damages whatsoever resulting from the use (or misuse) of information contained or implied in this leaflet. Please contact Guts UK if you believe any information in this leaflet is in error.