Overview
Indigestion (also known as dyspepsia) is a term used to describe unpleasant or even painful sensations at the top of the abdomen or in the lower part of the chest. Almost all of us are likely to experience indigestion from time to time, but it is rare that a serious underlying condition is the cause.
The symptoms of indigestion usually occur after eating or drinking. Indigestion is a symptom, not a disease and is so common that virtually everyone will experience it at some time.
Causes
Causes of indigestion
There are several different causes of indigestion, but it is rare that a serious underlying condition is the cause. Almost all of us are likely to experience indigestion from time to time, often after a heavy, spicy, or fatty meal. Sometimes symptoms occur when we have rushed our food or when we have simply had too much to eat or drink.
Functional dyspepsia
Functional dyspepsia is diagnosed when no specific cause of symptoms can be found. It happens when the nerves in the stomach become overly sensitive causing symptoms of pain. Eight in every ten people with indigestion are ultimately diagnosed with functional dyspepsia this is the most common cause of symptoms. Test results for a bacteria that can be found in the stomach called H pylori are usually normal, but this certainly doesn’t mean that the symptoms are not real. Some people with functional dyspepsia can have severe symptoms.
It is important that stress, anxiety, and depression are recognised as a possible cause. It is also possible that living with these symptoms longer term can affect people’s mood, too. The gut and the brain are connected, and this can cause stomach to become more sensitive to the normal signals that it sends to the brain (and vice versa). People with this diagnosis also might have other conditions diagnosed, an example is irritable bowel syndrome (IBS).
Ulcers
Although stomach and duodenal (peptic) ulcers used to be a common cause of indigestion they occur less frequently nowadays. Around 8 in 100 people with indigestion will have peptic ulcer disease, which is the second most common cause of indigestion. This is partly because most ulcers are caused by an infection called H pylori, and this bacterium (stomach bug) is becoming less common.
Some people are more prone to underlying conditions, such as peptic ulcer disease. This may be partly because ulcers tend to run in families. Ulcers are also more common in people who smoke and those who take one of the many non-steroidal anti-inflammatory drugs, for example aspirin or ibuprofen, for joint and muscle pains, as these can damage the stomach lining.
Other causes
Rarely, indigestion symptoms can be due to more serious conditions such as gallstones, diseases of the pancreas, or very rarely, cancer of the stomach but these will often have other symptoms as well. However, most people with indigestion don’t have any of these diseases and for most individuals who are diagnosed with functional dyspepsia, routine tests for these conditions are not required.
Symptoms
Most indigestion sufferers have their own pattern of symptoms, which range from mild discomfort in the upper part of the abdomen to quite severe pain. The pain sometimes might go through into the back. Some people may feel a burning sensation rising up in the chest called heartburn. While others experience a more general feeling of fullness (heaviness or bloating) and discomfort in the upper abdomen after a meal. Sometimes, a more localised painful sensation just below the breastbone is felt, or a combination of all three.
Indigestion can occur by itself or may be accompanied by other symptoms such as feeling sick (nausea), retching, or even vomiting, in rare instances. It appears to affect 1-2 in 5 people at any time, with around 1 in 4 people with symptoms visiting their GP for advice.
Does my indigestion need to be investigated?
Seek advice from your doctor if your indigestion does not settle with lifestyle changes or simple over the counter remedies. If you are feeling generally unwell or experience the following symptoms:
- Weight loss
- Persistent vomiting
- Problems swallowing
- Food getting stuck in your gullet
If you are having any other reason to think that there is a serious problem with your health, arrange to see your doctor as soon as possible. Plus, seek medical attention if symptoms start in middle age, or later, or if you have a strong family history of cancers of the stomach or gullet. Any signs of possible internal bleeding, such as vomiting blood or passing black tarry stools, is an emergency and means that you should seek medical advice without delay.

Having listened to your symptoms and examined you, your GP is likely to be able to reassure you that there is no serious underlying cause for your symptoms. Your GP can request a H pylori test on a blood or stool sample taken in the surgery. If diagnosed, a course of antibiotic therapy with an anti-acid drug can be prescribed by your GP. Your GP may also arrange a follow up test to make sure the H pylori infection has cleared up. However, if you are an older patient, aged 55 years or over, or someone whose symptoms are persistent or do not respond to treatment, your doctor may recommend that you undergo further investigations.
How likely is it that H.pylori is the cause of my indigestion?
Helicobacter pylori infection usually infects the lower part of the stomach (the antrum) and can cause inflammation of the stomach lining (gastritis).
There is good evidence that having a H pylori infection in your stomach increases your chance of having a peptic ulcer. H pylori is also possibly associated with functional dyspepsia. On the other hand, about half of people who have this infection don’t have any symptoms at all. It’s a good idea to have treatment for H pylori infection if you have it, even if the doctor can’t be sure if the infection is causing your symptoms. Getting rid of the infection will reduce your chance of ever having a stomach ulcer or a stomach cancer.
It is important to appreciate that clearing the infection does not always mean that you will stop having indigestion. Most people who have H pylori and functional dyspepsia are not going to see their symptoms cured by clearing up the infection.
What further tests might I be offered?
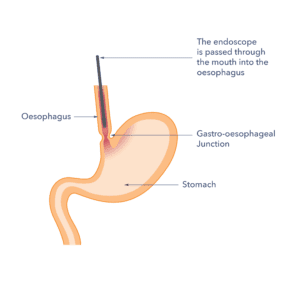
The most common investigation for those suffering with indigestion is an upper gastrointestinal endoscopy (known as gastroscopy for short), which is done as a day case procedure in hospital. This involves swallowing a thin flexible tube with a camera on the end so that the endoscopist can view the inside of your oesophagus, stomach, and duodenum and check for inflammation or infection. Although it is not pleasant, most people can tolerate just a few minutes of discomfort (the procedure is not painful) by having a local anaesthetic spray to the throat. If you are apprehensive or feel you have a sensitive throat, there are alternatives to make the procedure less uncomfortable, such as light sedation.
If you are being offered an endoscopy you should check that your doctor has first ruled out H.pylori infection or other conditions as the cause of your indigestion. If this is the case, then the doctor may feel that it is safest to check that you do not have a more serious condition which may only be picked up via endoscopy. The final decision whether to have an endoscopy is always yours. But it is worth considering that if you have a serious problem causing your indigestion a few minutes of discomfort during endoscopy is worthwhile to confirm this.
If you have symptoms of heartburn and reflux, for example a burning sensation, a sour taste in the mouth and your doctor diagnoses reflux disease.
Treatment
Treatment usually starts by looking for causes that can be remedied such as simple lifestyle changes. Lifestyle changes to consider include over-eating and weight gain, excess alcohol, smoking, rushed meals, eating too much fatty or spicy foods, having a healthy diet and regular activity plus avoiding smoking and drinking alcohol within guidelines are simple changes to try.
Some patients with indigestion can control their symptoms by taking over-the counter antacid tablets or liquids from the pharmacist. Some of these treatments work by neutralising stomach acid while others reduce the amount of acid your stomach produces. There are many products on the market, so it is worth discussing all the options with your pharmacist. Should simple medicines from the pharmacist be ineffective, your GP will be able to prescribe longer-term anti-acid or acid suppressing medication for you.
Your doctor will also be able to advise you about whether any other medications that you are taking are likely to be causing indigestion. Do not stop taking your medications without discussing it with your doctor first.
How can indigestion affect me over time?
Many patients with indigestion find that their symptoms improve either through self-help or after they have been investigated and treated by their GP. A small number, however, do go on to have longer-term symptoms, and they may find that they need to take treatment over a prolonged period. Finding the lowest dose of the medicine that keeps your symptoms at bay is a wise strategy. You may be able to have breaks between courses of tablets and just take your treatment when your symptoms are more troublesome.

For people who have longer-term indigestion associated with stress or anxiety, this can be treated by addressing the stress by seeking a referral to a psychologist for cognitive behavioural therapy or hypnotherapy. There are also medicines that can reduce the sensitivity of the nerves in the stomach, called neuromodulators. These are often used to treat people who experience mental ill health but in the context of functional dyspepsia are prescribed at a much lower dose to treat the stomach pain. Ask your doctor about this if you feel this is relevant to you.
Support
What to ask your doctor?
- How can I best self-manage my indigestion?
- Should I be checked for Helicobacter pylori infection?
- Do I need an endoscopy and if so why?
- What follow up or monitoring do I need?
Where can I get more information?
Guts UK has further information on:
Discover more:
Copyright © 2026 Guts UK. This leaflet was published by Guts UK charity in 2022 and is currently under review. The leaflet was written by Guts UK and reviewed by experts in indigestion and has been subject to both lay and professional review. All content in this leaflet is for information only. The information in this leaflet is not a substitute for professional medical care by a qualified doctor or other healthcare professional. We currently use AI translation tools on our website, which may not always provide perfect translations. Please check for further explanation with your doctor if the information is unclear. ALWAYS check with your doctor if you have any concerns about your health, medical condition or treatment. The publishers are not responsible or liable, directly or indirectly, for any form of damages whatsoever resulting from the use (or misuse) of information contained or implied in this leaflet. Please contact Guts UK if you believe any information in this leaflet is in error.

