Heartburn and Acid Reflux
Download printable versionOverview
Heartburn is extremely common, affecting up to 1 in every 4 of UK adults. Heartburn occurs when food or drink is consumed and the acid used to break down the contents in the stomach escapes and flows the wrong way up into the oesophagus.
Heartburn is a chest pain, often described as ‘burning’. It usually occurs after eating, lying down, or bending over. The pain is located at the lower end of the breastbone in the centre of the chest. The discomfort often rises upwards. Acid reflux is when some stomach contents, including acid, regurgitate into the gullet (oesophagus). It is the major symptom of gastroesophageal reflux disease (GORD). Reflux mostly occurs without us being aware that it is happening.
Causes
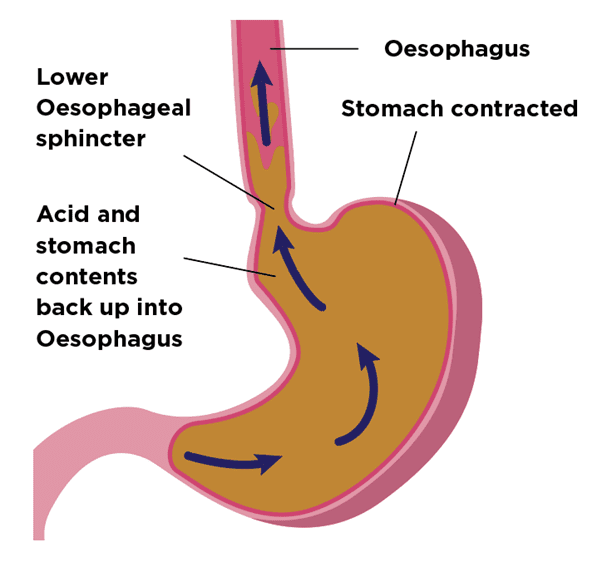
When food or drink is consumed, it passes from the mouth, down the gullet (oesophagus) into the stomach. A muscular ring called the lower oesophageal sphincter joins the oesophagus to the stomach. This ring should ensure that this flow is one-way. Acid reflux occurs when this one-way system does not work as well as it should do. This can allow your stomach’s contents to travel the wrong way, back up into the oesophagus.
The stomach makes acid. It aids digestion by breaking down food and drink. This is normal. Whilst the stomach can resist acid, if it refluxes in enough quantities into the gullet, it will cause pain. The pain is called heartburn. Sometimes the lining of the gullet can become inflamed (called oesophagitis). If the inflammation is severe, ulcers can form. Oesophagitis and ulcers would be seen at the time of an endoscopy.
Lifestyle factors: There are certain factors which appear to increase the risk of heartburn and reflux. These include:
- Smoking
- Drinking excess alcohol.
- Pregnancy
- Stooping or bending forwards.
- Having a higher than healthy body weight.
Pregnancy: During the later stages of pregnancy, some women may experience heartburn. This is because the growing baby puts pressure on the stomach, causing it to move upwards. The symptoms will often disappear once the baby is born but can continue afterwards.
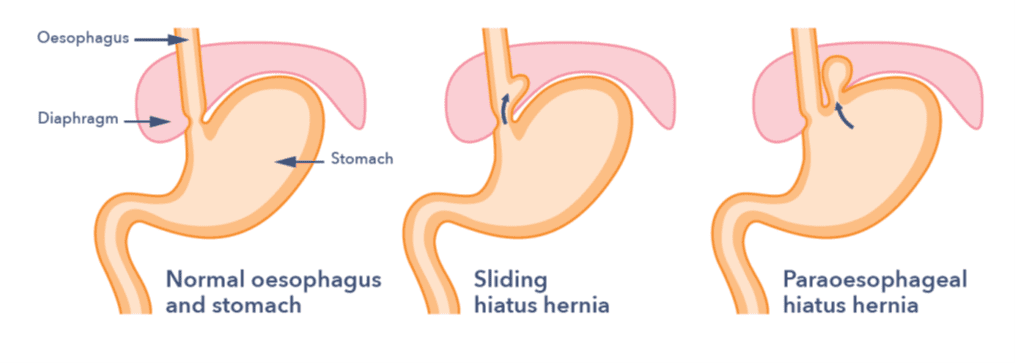
Hiatus hernia: This is when a part of the stomach moves upwards into the chest by passing through a hole in the diaphragm. The hole is known as the hiatus. This condition is called a sliding hiatus hernia or more rarely, a paraesophageal hernia. The hernia itself rarely causes any symptoms, but it does seem to make reflux more likely. For those people who have a large hiatus hernia, surgery may be required. Small hiatus hernias rarely require surgery.
Heartburn and reflux can sometimes be associated with other conditions such as Barrett’s oesophagus. It is common for people have reflux symptoms with a normal endoscopy. This can either be due to acid reflux not causing damage to the oesophagus or a condition where the oesophagus is overly sensitive to a normal amount of acid reflux.
Symptoms
Heartburn often worsens after eating rich foods, citrus juice, fizzy and hot drinks, or alcohol. However, for some, triggers can vary. Sometimes it can be felt deep in the chest, even in the back. In some cases, the burning sensation can extend all the way up to the throat. Some people notice acid reflux when some stomach contents “repeat.” They come back up the oesophagus to the throat or mouth. Some people might feel uncomfortable or have pain when they swallow. They might also need to clear their throat often, cough, or feel like they are choking. It is common for symptoms to be worse at night or when lying down.
Some people have slightly different, or ‘atypical’ symptoms of reflux. These might include voice changes, a sore throat, bad breath, a cough or problems with teeth that can be picked up by a dentist.
For most people with the condition, heartburn and reflux is just a nuisance and little more than that. For some, it can have an impact on day-to-day life. This can include interfering with physical activity and impairing sleep. In a few people where there is severe gullet inflammation, there is a risk of complications. These can include internal bleeding and narrowing of the gullet. One in ten people with acid reflux have Barrett’s Oesophagus. This is a condition that can, very rarely, progress to cancer of the lower oesophagus. If you are worried about these complications, discuss them with your GP.
You must always see your GP if:
- You have symptoms like food getting stuck in your oesophagus, frequently being sick or unintentional weight loss.
- Lifestyle changes and pharmacy medicines aren’t helping.
- You have heartburn most days for three weeks or more.
- You have difficulty or pain when swallowing food.
- You have heartburn, indigestion, hiccups or an unpleasant taste in your mouth for three weeks or more.
Diagnosis
Your doctor will ask about your reflux symptoms and how long you have had them. They might review the need for acid-reducing medicines. If the medicine doesn’t work or your symptoms come back, your GP may want you to have an endoscopy. This will ensure there are no problems with your oesophagus or stomach. Very commonly, people with reflux symptoms have only a little inflammation or their gullet looks entirely normal.
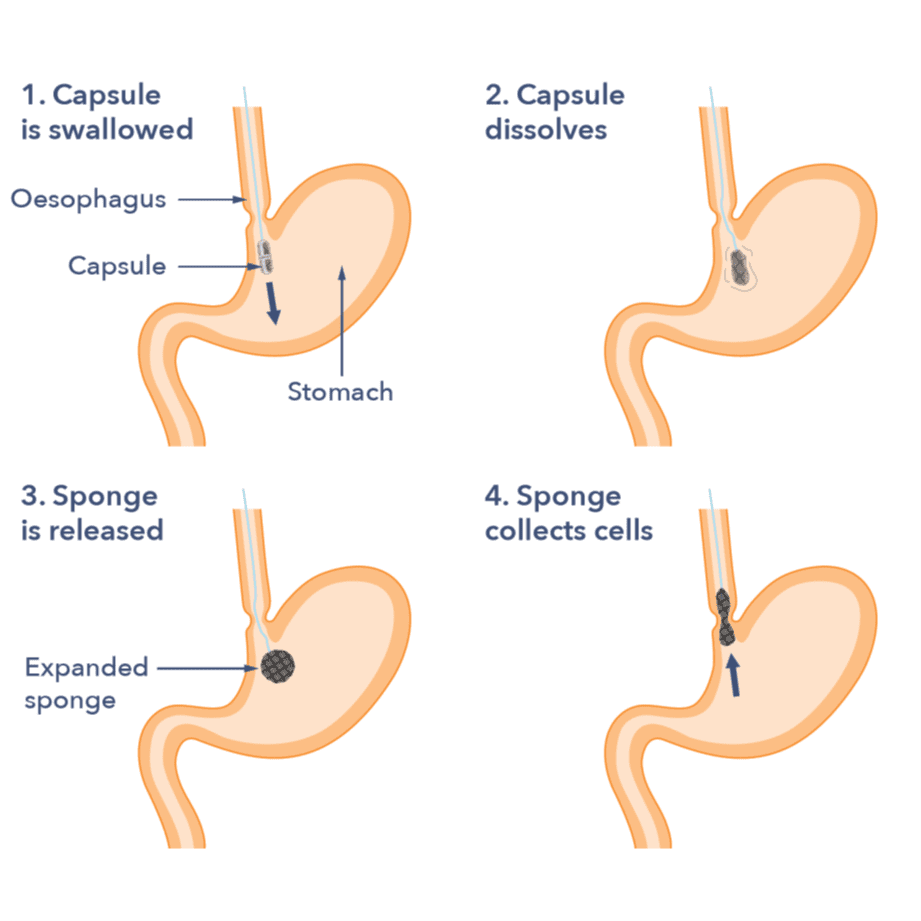
Capsule sponge test: This is a new test available in some parts of the UK. It might be a possibility if your doctor recommends you might need an endoscopy. It can help find Barrett’s oesophagus in people with ongoing heartburn and reflux symptoms. For the capsule sponge test you swallow a small capsule with a sponge inside, which is attached to a piece of thread. About seven minutes after swallowing the capsule, it dissolves in the stomach. Inside, there is a sponge that is released. A nurse removes the sponge by pulling on a thread. As the sponge comes out, it collects cells from the lining of the food pipe. These cells are then checked in a laboratory to see if there are any changes. More work is underway to find the test’s role in managing reflux and heartburn.
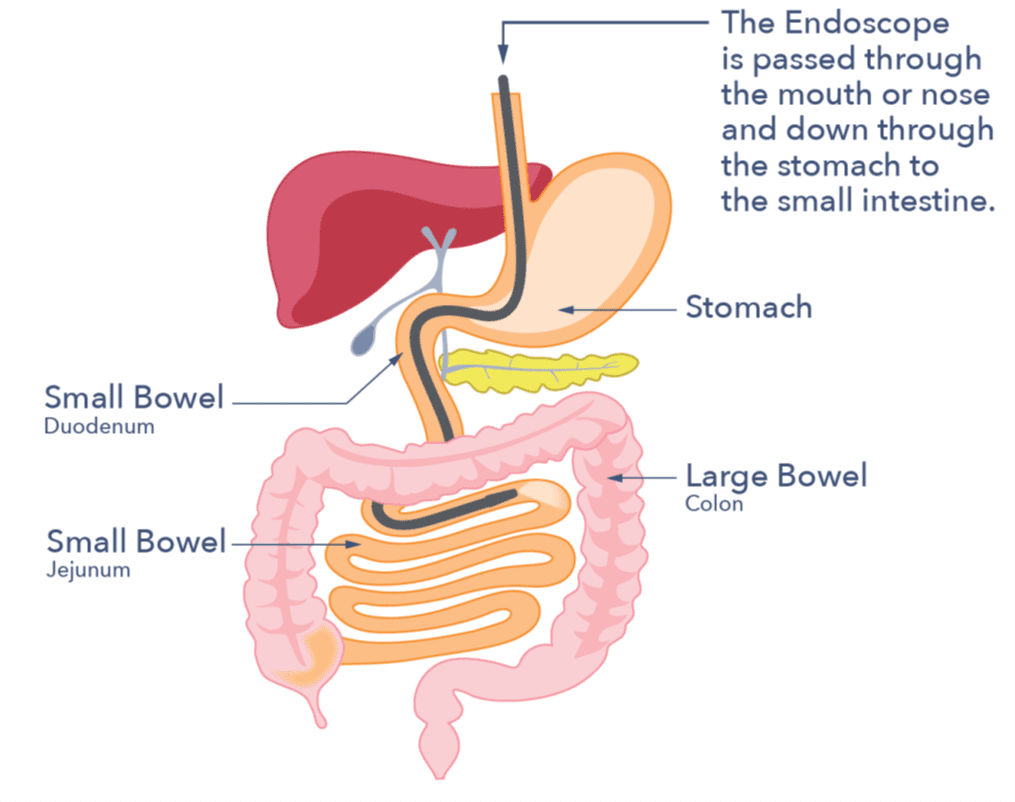
Endoscopy (gastroscopy): This is a test done at a specialist unit. It uses a thin, bendable tube. It goes through your mouth or nose and down into your oesophagus, stomach, and the start of your small intestine. It is usually carried out as an outpatient and takes less than 15 minutes. The endoscopist may take small tissue samples (biopsies) for lab analysis. You can choose to have a local anaesthetic throat spray and/or a sedative. The endoscopist can guide you in this decision. The procedure is not usually painful, but it may be uncomfortable at times. Ask your endoscopist for further information about the procedure.
Barium Swallow: An alternative to a gastroscopy is a Barium Swallow. It involves drinking a barium liquid and having X-rays. This will show up your oesophagus, stomach and first part of the small intestine on X-ray. It gives less information than an endoscopy but might be an alternative if an endoscopy cannot be done for any reason.
Treatment
Most treatments are lifestyle changes. Your symptoms are likely to lessen if you take measures to reduce the amount of reflux that you have. For example, quitting smoking and reducing alcohol can help a lot. Your GP will treat you for H Pylori if the test is positive.
Alcohol: Check your alcohol intake. Reduce it, if needed, to within healthy limits. If you have a large intake, discuss it with your GP before reducing it. Use this online calculator to check your alcohol units: drinkaware.co.uk. Health advice is not to have more than 14 units per week with some alcohol-free days during the week.
Smoking: Ask your GP about NHS stopping smoking services where you live. There are many different methods to use and stopping can have other benefits to health. See here for more information www.nhs.uk/live-well/quit-smoking.
Diet: Some foods are more likely than others to trigger reflux symptoms. Cutting down on fizzy drinks may help reduce symptoms, although it hasn’t been proven conclusively. It’s been shown that drinks containing caffeine (such as tea, coffee, and some energy drinks) can cause heartburn. Evidence is again inconclusive with respects to the benefits of reduction. People can find that spicy food, food higher in fats and tomato are more likely to trigger symptoms. Reduction of these foods might be helpful. There is no one approach to diet and reflux and triggers can be very individual. The NHS has a helpful video on diet and lifestyle with reflux which you can watch below.
Having a higher weight than is considered healthy: Having a higher weight can put more pressure on the stomach. This makes reflux episodes more likely. Review your weight, as excess body weight can create upward pressure from the stomach. If you have a higher than healthy weight, it can be helpful to take steps to reduce it. You can speak to your GP about the weight management services that are available in your area. You might also find this NHS free weight loss programme useful at nhs.uk/live-well/healthy-weight.
Eating patterns: You may find it helpful to look at how you eat as well as what you eat. The way that you eat might help to reduce symptoms.
- Avoid late-night, high-fat meals so you don’t go to bed with a full stomach. Eat your main evening meal at least three hours before going to bed.
- Reduce late-night snacking if this applies to you. Do not skip breakfast.
- Eating meals too quickly can cause symptoms. Chew each mouthful well before swallowing your food.
- Eating beyond fullness, for example, eating large meals. Eat little but more often, if necessary.
- Try to avoid bending forward or wearing tight clothes as this can put extra pressure on your tummy.
Sleeping position: Sleeping on your left side can help. Or, for people who lie flat, using a wedge pillow or elevating the head of the bed or mattress by up to 20cm can help. This approach may reduce nighttime symptoms by making it less likely for the acid to enter the gullet. Using extra pillows is not recommended.

There are also a variety of medicines you can buy at your local pharmacy to help lessen your reflux symptoms:
Antacids: Alkaline liquids or tablets that reduce the amount of stomach acid. They usually work immediately. They are best taken after meals and before going to bed.
Alginates: These are products that form a thick protective layer on top of the stomach contents and help reduce reflux symptoms. These can be useful to take after meals and before going to bed to reduce nighttime symptoms. Some medications are a combination of both antacids and alginates.

Acid-suppressing medications: These are capsules or tablets which reduce the amount of acid produced by the cells in your stomach.
These are split into 2 groups:
- Histamine H2-receptor antagonists (H2 blockers): These include cimetidine, famotidine and nizatidine. These can be taken before bedtime.
- Proton pump inhibitors (PPIs): They include omeprazole, lansoprazole, pantoprazole, rabeprazole, and esomeprazole. These are best taken 30 minutes before breakfast or evening meal.
The most effective therapies are Proton Pump Inhibitors (PPIs) in managing symptoms of heartburn and reflux. These are remarkably safe and among the most commonly taken medicines worldwide. Using these medicines long-term may cause issues. They may increase the risk of bowel infections and bone fractures. However, these drugs are generally safe and very effective at controlling reflux.
Your doctor may first prescribe up to 8 weeks of a PPI, depending on how severe your reflux is and how quickly the symptoms reduce.
It is recommended that PPIs are taken for the shortest time at the lowest dose. So your doctor may advise coming off the medication. If your symptoms return, the doctor may lower your dose to the lowest level that manages them. Speak to your GP, pharmacist, endoscopist or gastroenterology specialist. They will be able to discuss with you any concerns you have about your acid medication.
For some conditions confirmed by endoscopy, there are exceptions. In those cases, it may be suggested you stay on these medications long-term. These are:
- Severe gastro-oesophageal reflux disease (GORD).
- An oesophageal stricture (narrowing).
- Barrett’s oesophagus
Surgery: Several types of surgeries are available in some circumstances. Examples of these include when lifestyle changes fail. Or when you cannot tolerate or do not want to rely on medication long-term.
Laparoscopic fundoplication is the most common type of surgery: It is a keyhole surgery performed under general anaesthesia. It aims to reduce reflux by folding and stitching the top of the stomach, creating a smaller opening. This surgery might resolve your reflux, but it does come with short-term complications. During the initial weeks of recovery, you may feel some pain and have difficulty swallowing. To manage this, you will need to follow a diet consisting of pureed and soft foods. The hospital staff where you have your surgery should advise you about the diet you need. Ask your doctor about the risks and benefits of this surgery for your situation.
Laparoscopic insertion of a magnetic ring around your oesophagus, the LINX procedure. It is performed under general anaesthetic. The magnetic force of the beads reduces reflux, but it is weak enough to allow swallowing. For a few weeks after the surgery, you might have trouble with swallowing. In some cases, you need an endoscopy and dilatation. This is to stretch the narrowed area of the oesophagus. Sometimes the reflux might return and then the band will have to be removed. You will remain eligible for most MRI scans. But the band might need to be removed if you need to undergo a high-strength MRI scan. Ask your doctor about the risks and benefits of this surgery for your situation.
There are other types of surgery being investigated for heartburn and reflux. Although the evidence for using these treatments is currently limited.
Support
Does heartburn and acid reflux need to be monitored and, if so, how?
Many people find that their symptoms improve greatly if they change their lifestyle. Others may need to take medicines from time to time or long-term, depending on the results of an endoscopy. There are some people for whom drug treatment is not suitable for one reason or another. In such cases, your GP may then refer you to your local hospital’s Gastroenterology Department for their advice. In some cases, like when anti-reflux surgery is needed or medicine hasn’t helped, you may need pH testing. This testing happens at a specialist physiology department in the hospital. The pH test uses a thin, flexible tube through your nose and into your gullet to check for acid reflux. It tracks acid reflux all day as you go about your usual activities. This links to a small recording device you carry while testing.
What to ask your doctor?
- Do I need an endoscopy?
- What can I do in terms of my lifestyle to reduce gastro-oesophageal reflux?
- How should I take my medications?
Where can I get more information?
The following are charities who you can contact to find out more information:
We’re getting to grips with guts!
Guts UK is the national charity for the digestive system. Our guts have been underfunded and misunderstood for too long. Together, we can change that.
Please consider donating to us today to help us help the next person who needs our support. Guts UK funds life-changing research, empowers people to seek help so no one suffers in silence, and provides expert information for people affected by digestive conditions. Together, let’s help the UK get to grips with guts.
Discover more:
Copyright © 2026 Guts UK. This leaflet was published by Guts UK charity in September 2025 and will be reviewed in September 2028. The leaflet was written by Guts UK and reviewed by experts in heartburn and reflux and has been subject to both lay and professional review. All content in this leaflet is for information only. The information in this leaflet is not a substitute for professional medical care by a qualified doctor or other healthcare professional. We currently use AI translation tools on our website, which may not always provide perfect translations. Please check for further explanation with your doctor if the information is unclear. ALWAYS check with your doctor if you have any concerns about your health, medical condition or treatment. The publishers are not responsible or liable, directly or indirectly, for any form of damages whatsoever resulting from the use (or misuse) of information contained or implied in this leaflet. Please contact Guts UK if you believe any information in this leaflet is in error.




