Overview
This information helps to explain the symptoms of constipation and what causes them. It will help you to identify when it is a problem needing your doctor to investigate it. The information also highlights what treatments are available to help reduce symptoms.
Constipation is a symptom that can mean different things to different people. The usual meaning is that a person has difficulty or infrequency with opening their bowels. Constipation affects around 1 in 7 otherwise healthy people with young women designated female at birth and older people being two groups most likely to experience constipation. Constipation is a problem for some people who need to take medicines. Examples include morphine and codeine. These are called opioid based medicines.
There is a common belief that people need to open their bowels every day, but this is not the case. Opening bowels can vary between three times a day to three times a week in healthy individuals. Constipation is a common problem and does not usually mean that anything is seriously wrong. Most people’s constipation is temporary and will clear up with simple lifestyle measures.

How do you know if you have constipation?
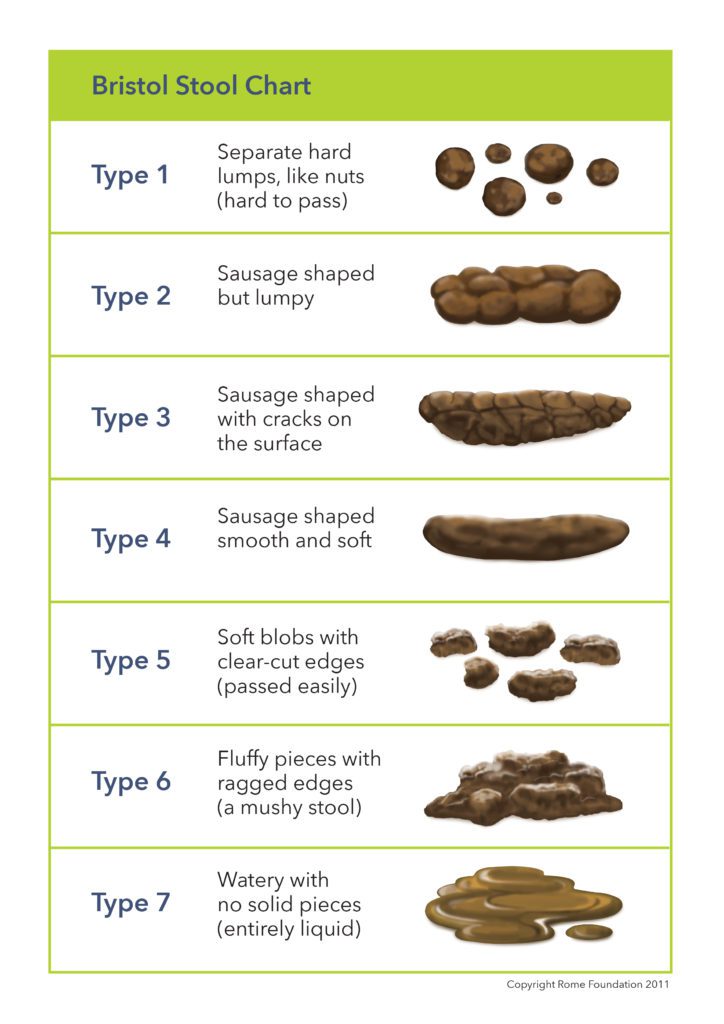
This chart, called the Bristol Stool Chart, is a way of identifying constipation. Constipation generally refers to poo that is type 1 or type 2 on the chart. The poo is often hard and difficult to pass.
Causes
Medicines
Medicines can often cause constipation as a side-effect. Opioids are one of the commonest types of medication that can cause constipation. It is important to talk to your doctor if you feel your constipation started or was worsened by taking a medicine. Don’t stop taking a medicine without seeking medical advice. Your doctor may give you an alternative medicine. Please see Guts UK information on painkillers causing constipation for more information or contact 020 7486 0341 for a copy.
Emotion
There is a strong connection between our brain (including our mood) and the way the gut works. This is called the gut-brain connection. The brain and gut ‘talk’ to each other in many ways for example, via hormones or nerves. Examples of normal signals are:
- Feeling hungry (gut talking to brain).
- Feeling butterflies (brain talking to gut).
Sometimes the brain and gut overshare information. Being upset or depressed can make the bowel slow down or speed up.
Ignoring the natural urges to open bowels
Ignoring bowel urges can change both how the bowel muscles work and the pattern of bowel opening. This happens due to inadequate time, an aversion to public toilets, or social limits. This situation can also be caused by pain, or fear of pain, on passing poo. This can happen in case of an earlier presence of a small tear (anal fissure) or piles (haemorrhoids).
Menstrual constipation
Those designated female at birth may notice that their bowels are slower at certain times of their menstrual cycle.

Disordered eating behaviour
People who eat irregularly may be more prone to constipation. Constipation is a symptom of eating disorders. Examples include bulimia nervosa or anorexia nervosa. The constipation can continue after the disordered eating behaviour stops.
Low physical activity
Among people with a susceptibility towards constipation, low activity might worsen symptoms.

Pelvic floor weakness
Some people can develop a weakness of the pelvic floor. This results in the bowel bulging abnormally during rectal emptying. Doctors call this a rectocele. A large rectocele can interfere with the emptying mechanism. This can be especially common in those designated female at birth who have had children.
Dilated bowel
This is a less common condition in which the bowel becomes abnormally large (dilated). It is called a megacolon or megarectum, which can be a cause of constipation. People normally have symptoms of severe constipation, bloating and pain. A bowel obstruction needing hospital treatment can occur. You should contact your doctor if you are having these severe symptoms, are unable to pass wind and being sick.
Why does constipation occur?
There are three main mechanisms that may cause constipation:
- One mechanism is where the muscles lining the gut wall do not work properly. This results in the sluggish movement of contents through the bowel down to the rectum. It leads to a reduced urge to empty the bowel and hard poo. People have an infrequent urge to go to the toilet. This is called slow transit constipation.
- Another mechanism of constipation is where the muscles lining the gut wall work. But people still have constipation symptoms, this is the most common type of constipation. It is called normal transit constipation. Normal transit constipation and irritable bowel syndrome with constipation (IBS) have considerable overlap.
- A defaecatory disorder is another cause of constipation. This is where a person has difficulty evacuating their bowels despite excessive straining. It is due to a problem with muscles that line the pelvic floor. People with a defaecatory disorder may have normal transit or slow transit constipation.
Symptoms
The main symptoms of constipation are:
- Opening the bowels less than three times a week.
- Needing to strain to open your bowels on more than a quarter of occasions.
- Passing a hard or pellet-like stool on more than a quarter of occasions.
- Experiencing a sense of incomplete emptying after a bowel opening.
- Needing to use manual manoeuvres to achieve bowel emptying. For example, some people insert a finger into the anus to stimulate a bowel motion (digitation). Others press on the pelvic floor area to help empty their bowel.
Constipation does not have a single symptom and it can refer to one or more of the above features. The more of these symptoms you have the more likely you are to have constipation. If abdominal pain is also a symptom, the constipation may be due to IBS. (see our separate booklet). Abdominal bloating is often part of many bowel complaints, including constipation.
Constipation is bothersome but usually not serious. If simple measures described later don’t help and your symptoms persist, then contact your GP. Also, report any sudden slowing up of your bowel, especially if you are over 40, to your GP.
If you also experience any of the following symptoms, you should see you GP immediately:
- Unexplained weight loss.
- Bleeding in the stool (nhs.uk/conditions/bleeding-from-the-bottom-rectal-bleeding)
- Or rectal pain.
Your doctor will diagnose you according to the number or severity of symptoms as above. They may also want to feel your belly to check for any tenderness or swelling. Further investigations are usually not required. But this will depend on your symptoms, age, and whether you have a family history of bowel problems. If your doctor has any concerns, they may request one or more of the following investigations:
- Blood tests: These are usually to look for anaemia or metabolic problems. For example those that may be related to diabetes or the thyroid.
- A poo test called FIT test: To see whether there is hidden blood loss in your poo.
- Flexible sigmoidoscopy, colonoscopy, or CT scan: These are tests which allow doctors to study the lining of your bowel. They are routine procedures which are safe to perform in most cases. Bowel preparation is required before these procedures. Which would be explained further by your doctor or nurse if needed.
- Transit studies: A test involving an x-ray which shows the speed of markers as they pass through the bowel. Laxatives cannot be taken during the test.
- Anorectal physiology testing (anorectal manometry and balloon expulsion test) and proctography: These tests are rarely carried out. They are mostly performed in specialist neurogastroenterology centres. The tests help visualise the structure of the pelvic floor and the nerves and muscles around the back-passage. It also shows how they work. Bowel preparation is not always required. These tests could be requested by a consultant after the above tests have not shown the problem.

Treatment
People can be greatly concerned about being constipated. Consider if you have had a change in circumstance recently to cause the problem. For most people, constipation can be self-managed. Treatment is generally orientated around lifestyle changes:
Dietary changes
Regular meals and a good fluid intake are the main lifestyle changes in preventing and treating constipation. For the average adult eight mugs or tall glasses of fluid a day is a normal amount to drink. Some people find that drinking drinks including caffeine (particularly coffee) can help the bowel open.
A high fibre diet
This may help some patients with constipation. This should include a mixture of high fibre foods. Examples are:
- Fruit.
- Vegetables.
- Nuts.
- Wholemeal bread and pasta.
- Wholegrain cereals and brown rice.
Aim to include a high fibre food at each meal along with at least five portions of fruit or vegetables each day. Some people may find that it helps to eat more fruit and vegetables while others might prefer cereals and grains. Including more fibre may lead to bloating and can worsen discomfort at the start of treatment. So, it is important to increase levels slowly. Fibre is most helpful for people with mild symptoms of constipation. But, if constipation is severe, please consult your doctor before continuing to increase your fibre intake. Continuing to increase fibre may occasionally make symptoms worse.
See our information here on fibre.
If you have IBS the advice may be different, the British Dietetic Association has a fact sheet.
If you are struggling with your diet, ask your GP for a referral to a dietitian.

Listening to your body
A good bowel routine is important. Plan a place and time of day when you are comfortably able to spend time in the toilet. Respond to your bowel’s natural pattern so when you feel the urge, don’t delay.
Exercise
Keeping active and mobile may help some people whose bowel is sluggish.

Should I take laxatives and are they safe?
Regular use of laxatives is generally not encouraged but occasional use is not harmful. The balance of scientific evidence suggests that laxatives prescribed by a doctor do not cause long-term damage to the bowel.
There are many different laxatives. They tend to work in one of two ways. Stool softeners draw water from the body to soften the poo. Stimulant laxatives stimulate contractions (movement) in the bowel to help the bowel release the poo.
Taking laxatives does not result in weight loss. They work on the large bowel and most of the goodness from food is absorbed in the small bowel. Commercial products containing laxatives such as ‘weight loss’ or ‘skinny’ tea are available. These products do not result in weight loss and so are not advised to be used. Taking laxatives that are not prescribed by a doctor can be harmful.
If an eating disorder is the reason that you are taking large amounts of laxatives, talk to your GP.
Further treatments
If you have tried laxatives and diet changes, and you are still constipated, ask your doctor about:
- Medicines: Newer medicines can be helpful for some people who don’t tolerate or don’t respond to simple laxatives. Newer laxatives include prucalopride and linaclotide. Prucalopride is a medication that improves the movement of the bowel. Linaclotide is a medication that increases the secretion (water) and reduces the sensitivity of the bowel.
- Biofeedback: This involves training to help the person co-ordinate rectal and abdominal muscles better. The technique uses weak electrical signals to help you recognise how your body functions and help you to change the muscles movement. This helps the bowel empty more effectively. Treatment is available in some hospital centres.
- Behavioural treatment such as Cognitive Behavioural Therapy (CBT) and hypnotherapy: These treatments have been found to be useful in patients with IBS including IBS-C. No studies are available in chronic constipation without IBS.
- Transanal Irrigation: This is a treatment that may be helpful for people with chronic constipation. The equipment, or catheter, flushes water into the rectum to help emptying. Training from a healthcare practitioner is provided in how to use the equipment yourself. It can take several weeks to get used to using the equipment. Do not be tempted to use irrigation by yourself without training and don’t use colonic alternative therapy. Availability of this treatment may vary.
- Surgery: Surgery is very rarely considered in the treatment of constipation. There are some people who develop new symptoms after an operation e.g., diarrhoea, bowel obstruction or incontinence. Pelvic floor surgery may be helpful for conditions like large rectocele (a weakened area in the wall of the bowel) and rectal prolapse (where the rectum sags through the anus). This surgery would need a specialist assessment from a surgeon to decide what requires repairing.
Any sudden change in your symptoms should be reported to your doctor.
Complications
How can constipation affect you?
Although constipation can be worrying, there is no reason to think that constipation can ‘poison’ the body. It can cause feelings of sluggishness and bloating. There is no evidence that toxins leak from the bowel into any other part of the body. Another common idea is that constipation may lead to cancer. There is no convincing evidence that long-term constipation increases the chance of bowel cancer.
Remember that most cases of constipation are easily solved with simple diet, lifestyle, or medication change. But if constipation does not respond to treatments there can be medium to long term complications. These include:
- Haemorrhoids or fissures: Bleeding from haemorrhoids, or more rarely, a painful tear at the anus, are common in patients with constipation.
- Rectal prolapse: Excessive straining can lead to the rectal wall protruding out through the anus.
- Faecal impaction: This is a build-up of poo in the rectum that can occur in people who are older, immobile or have a severe impairment of bowel movements. This needs prompt treatment by either their GP or hospital.
Support
What to ask your doctor?
- Could any of my medications be causing my constipation and if so is there an alternative?
- What dietary or lifestyle changes do you suggest I introduce?
- Are laxatives suitable for me and if so which one would be best for me to use?
- How will my constipation be monitored?
- Are there any over the counter remedies which will reduce the chances of me getting haemorrhoids or an anal tear?
Other resources
The What’s Up With My Gut website makes the process of diagnosis easier to understand and less overwhelming, with step-by-step guides to support you to understand the actions your GP might take. This can help you to get the best out of your GP appointments and understand which conditions your GP might look into and what tests or investigations they might consider.
Discover more:
Copyright © 2026 Guts UK. This leaflet was published by Guts UK charity in 2023 and will be reviewed in 2026. The leaflet was written by Guts UK and reviewed by experts in constipation and has been subject to both lay and professional review. All content in this leaflet is for information only. The information in this leaflet is not a substitute for professional medical care by a qualified doctor or other healthcare professional. We currently use AI translation tools on our website, which may not always provide perfect translations. Please check for further explanation with your doctor if the information is unclear. ALWAYS check with your doctor if you have any concerns about your health, medical condition or treatment. The publishers are not responsible or liable, directly or indirectly, for any form of damages whatsoever resulting from the use (or misuse) of information contained or implied in this leaflet. Please contact Guts UK if you believe any information in this leaflet is in error.




