Diverticular disease
Download printable versionOverview
This factsheet is about diverticular disease of the large bowel (colon).
Diverticular disease is a diagnosis given in people who have symptoms and is extremely common in the developed world. Between 1 in 3, increasing to 1 in 2 people will be affected during their lifetime. Slightly more females are diagnosed than males in the UK.
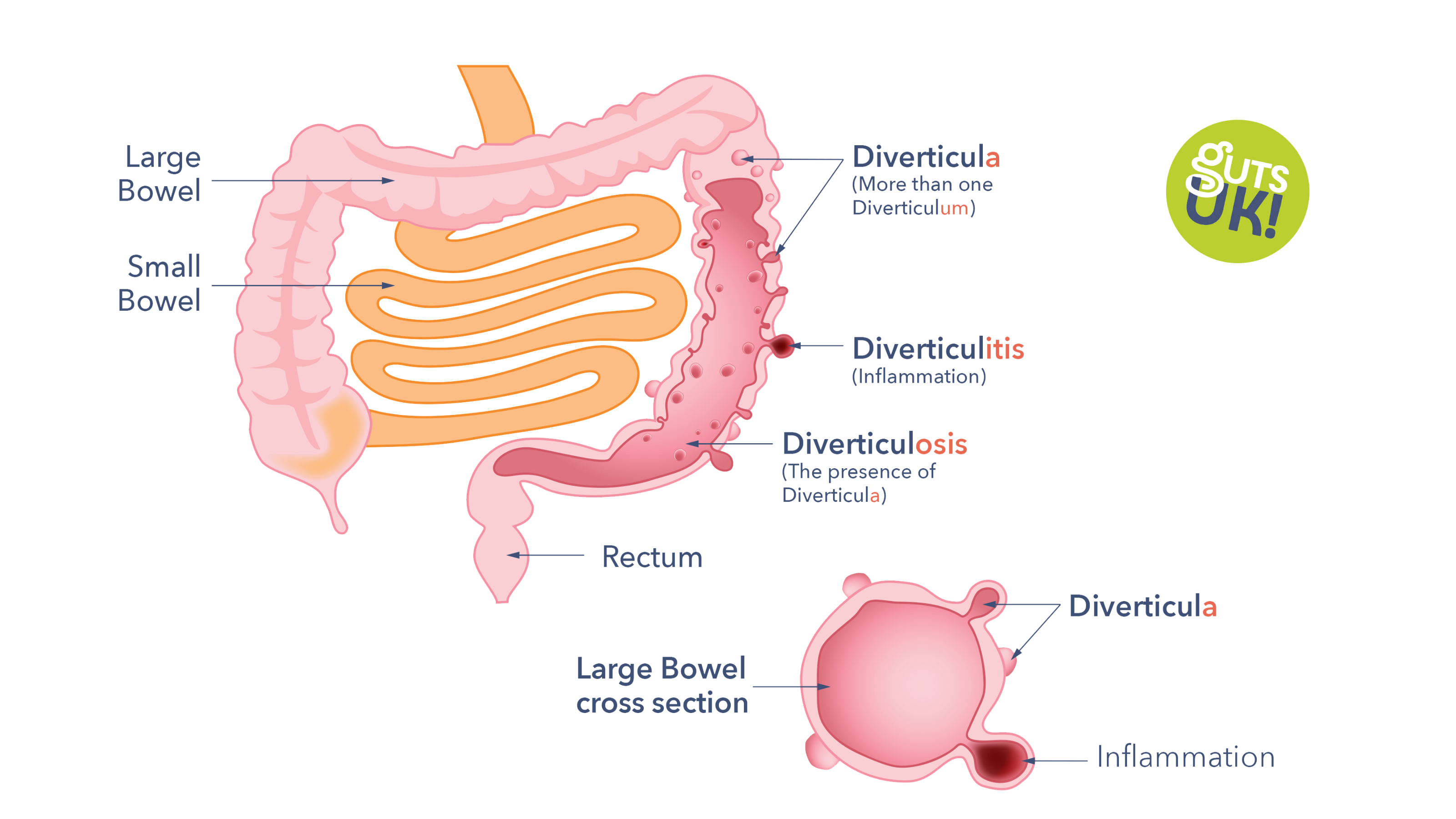
What does diverticular disease look like?
- Diverticulum: A diverticulum is a small pouch about 1cm in size which sticks out from the wall of the large bowel.
- Diverticula: This refers to more than one Diverticulum. The most common site for diverticula is on the lower part of the large bowel on the left-hand side. They are permanent unless the affected part of the bowel is surgically removed.
- Diverticulitis: Diverticulitis means the condition that occurs when a single diverticulum or several diverticula become inflamed or infected.
- Diverticulosis: You may have heard the term diverticulosis, which means the presence of diverticula, this is not the same as diverticular disease. Most people with diverticulosis do not have, or go on to develop, diverticular disease. The great majority of people with diverticulosis will live out their lives never having symptoms. Having symptoms is diagnosed as diverticular disease.
Causes
What causes the development of diverticula?
The short answer is that it is still uncertain what causes diverticula to develop. The most important risk factor is age. After the age of 40 they become more common. With increasing age about 2 out of 3 people will develop diverticula during their lifetime. More people are being diagnosed, especially people under 45 years of age.
A lot of interest has been placed in lifestyle factors. Diverticula are commoner amongst people with an unhealthy high body weight. Current data is conflicting for fibre intake and risk of developing diverticulosis. A recent study suggests that a higher intake of fibre and vegetables lowers the risk of developing diverticulosis, but other studies do not show the same results. The idea that constipation causes the development of diverticula has also not been proven to be correct. Diverticular disease is associated with people who have a diagnosis of Ehlers Danlos Syndrome, Williams Syndrome, and polycystic kidney disease. This is because these are diseases that occur in families and can affect the tissue make-up of the bowel.
> Learn how to increase your fibre intake
Diagnosis
How is diverticular disease diagnosed?
Diagnosis is made by examination of the inside of the large bowel. During the examination the doctor or nurse endoscopist will be looking for other abnormalities that could be causing your symptoms. Diagnosis is only confirmed once other conditions have been ruled out. This can be done via:
Colonoscopy or sigmoidoscopy
A tube with a camera is passed into the large bowel via the back passage to view the inner surface of the large bowel. A sigmoidoscopy is a similar procedure that views less of the large bowel. Medicine can be given to make the procedure more comfortable. You will be given medicine to make you poo before the procedure. This ensures you completely empty your bowels. This medicine will cause diarrhoea and urgency; therefore, it is a good idea to stay near a toilet.
CT scan
This is a non-invasive x-ray-based test although, as with the colonoscopy, you will be required to completely empty your bowels before the scan.

Symptoms
How can diverticular disease affect you?
It is important to remember that most people with diverticular disease will never have any complications and can carry on with their lives as normal.
Symptoms
The most common symptoms include:
- Lower abdominal pain
- Bloating (increase in abdominal size due to gas)
- Change in bowel habit (diarrhoea or constipation)
- Mucus or blood in the stool
The pattern of symptoms differs from one person to the next, but pain is often
crampy, and it comes and goes. The pain is commonly focussed in the left side of the abdomen (belly) where the diverticula most often occur. In a small number of people, and people of South Asian origin, symptoms may occur on the right-hand side of the abdomen. Pain and bloating can often start after food is eaten and may ease when a stool or wind is passed. Many people experience a change with diarrhoea one day and constipation the next.
It is important to remember that many symptoms of diverticular disease are very similar to those of more serious conditions such as bowel cancer so do not assume that they are due solely to diverticular disease.
If you experience a change in symptoms or develop new symptoms , especially
blood in your stools, consult your doctor. Your doctor may want to check you over
to make sure something completely unrelated to diverticular disease was not
developing instead. The reason for this is that symptoms of diverticular disease may overlap with conditions such as irritable bowel syndrome (IBS), colitis and cancer.
Complications
Relatively few patients ever get complications severe enough for them to be admitted to hospital and very few people die of this very common disease. However, in some cases, complications can occur, and these include:
Inflammation (Diverticulitis):
This is the most common complication, occurring between 1 in 10 to a quarter of people with the condition. More people are being diagnosed, particularly in individuals under 45 years of age. In people over the age of 50, acute diverticulitis happens more frequently in females. In those under 50 years of age, it occurs more commonly in males. The current theory is that the inflammation and/or infection occurs because of an overgrowth of bacteria in the diverticula.
Symptoms of diverticulitis:
- Worsening abdominal pain.
- High temperature.
- Nausea (feeling sick) or vomiting (being sick).
If any of these symptoms are experienced, medical help should be sought immediately. Complicated diverticulitis requiring hospitalisation is normally treated with antibiotics (germ killing medicine) and fluids.
Sometimes, when infection is severe, it can cause further complications such as:
- A collection of pus (abscess).
- An obstruction (blockage of the bowel).
- Or a perforation.
If these complications arise, an operation to remove part of the large bowel, or a needle placed into the collection of pus to drain it may be needed.
Blockage of the gut:
Scar tissue can sometimes form around the inflamed diverticulum. This may lead to narrowing of the colon, which can cause a blockage.
Perforation:
Sometimes an inflamed pouch (diverticulum) can burst, causing a hole in the wall
of the bowel. A perforation can lead to peritonitis, a serious condition with
widespread inflammation in the whole of the abdomen.
Bleeding:
A blood vessel in the wall of a diverticulum can rupture leading to bleeding into the large bowel. 1 in 3 people with bleeding as a symptom can have a severe episode of bleeding requiring hospital admission.
Fistulas:
Rarely, the presence of diverticula may lead to formation of abnormal connections or tracts (fistulas) between the gut and other organs such as the bladder or vagina. Signs of this include small amounts of stool in the urine or foul-smelling discharge from the vagina. If diagnosed, surgery is usually necessary, so it is important to see a doctor if you have these symptoms.
Treatment
What treatment is available for diverticular disease?
The causes of flare-ups of diverticular disease or the development of complications such as acute diverticulitis is unknown, despite research. Following the diagnosis of diverticular disease, many people will ask their doctor for advice on how to prevent development of complications.
Diet:
You are advised to eat a healthy, balanced diet including whole grains, fruit and vegetables. This involves eating lots of different healthy foods. The aim is to have a fibre containing starchy food with each meal. Plus five portions of fruit and/or vegetables per day. Try to drink at least two litres (eight to ten cups) of fluid every day to help the fibre pass through the bowel. A portion of fruit and vegetables is 80g (or a handful). Smoothies are 150ml portion as they generally contain a lower amount of fibre. If you don’t have much fibre in your diet or suffer from constipation it is important to increase your intake slowly. This will to avoid symptoms of bloating and wind, it may take some time for improvements to be seen to constipation symptoms. There is no need to avoid seeds, nuts, popcorn or fruit skins.
| Starchy foods | Wholemeal, brown or granary bread. Oat or rye bread. Wholegrain crackers, wholegrain rice and wholegrain pasta. Wholegrain breakfast cereals, wheat bisks and non wholewheat options such as oats, museli and gluten free wholegrain cereals.Chapatti or naan bread made with wholegrain flour. |
| Fruit | All varieties are suitable including fresh, frozen, dried and canned. |
| Vegetables | All varieties are suitable including fresh, frozen, dried and canned. Vegetable soup. |
| Protein containing foods | Chickpeas, lentils, peas and beans, dhal.
Nuts and seeds. |
| Desserts and other snacks | Puddings containing dried fruit, oat-based crumble toppings, biscuits containing wholegrain flour, nuts, dried fruit and seeds, flapjack, muesli bars and fruit bars based on dates.
Chocolate containing nuts and dried fruit, root vegetable crisps. |
| Drinks | Smoothies and milk shakes containing the whole fruit. (150ml portion size. One portion per day counts as one of your 5 fruit and/or vegetables per day). |
If you also have been diagnosed with irritable bowel syndrome (IBS), increasing
wheat bran fibre intake can make symptoms worse for some people. Therefore if
symptoms continue, increase bran fibre intake using non-wheat bran alternatives
(e.g. oat, rice). These are generally better tolerated alternatives.
If you change the type of food, you eat it is important to ensure your diet remains balanced and nutritious. The NHS website has useful information on what constitutes a healthy diet. It also contains the Eatwell Guide, a visual representation of which food groups you need to eat, and in what proportions, to achieve a balanced diet. The British Dietetic Association also has useful information on healthy eating on their website.
Go through to Guts UK’s Healthy Eating & The Digestive System information here.
If you experience any of the following you can ask your GP or consultant for a referral to an NHS dietitian:
- You have any other restrictions to your diet for other diagnosed medical conditions.
- You are having problems with regards to knowing what to eat.
- You have continuing symptoms of gas, bloating and diarrhoea.
You should see your doctor if you have any changes in symptoms.
You should take regular exercise, lose weight if you are overweight or obese, and stop smoking. However the studies on which these recommendations are made are not highly definite for reducing the risk of developing a complication from diverticulitis. These changes to a person’s lifestyle will bring additional wider benefits in general health and wellbeing.
There are variable results from the use of probiotics (good bacteria) to prevent diverticular disease progressing, so use of probiotics cannot be advised at this time.
Medications:
There is no specific medical treatment for the general symptoms of diverticular disease although if you have been experiencing constipation, check with your pharmacist or doctor if the use of a bulk-forming laxative might help. Painkillers such as codeine should be avoided as they tend to worsen and can even cause constipation, a pharmacist can provide advice with regards to alternatives for abdominal pain. Read more about painkillers causing constipation here. For diverticulitis your doctor may adopt a ‘watch and wait’ approach and may consider antibiotics for those who are unwell, have a compromised immune system or other relevant long-term conditions. Tell your doctor immediately if your symptoms become worse in this situation. See the section on inflammation (diverticulitis) for symptom information.
Surgery:
This is usually only done after an episode of inflammation because an abscess has formed around the large bowel, or infection from the inflamed perforated diverticulum has spread more widely within the abdomen. The commonly performed operation cuts out the segment of the bowel with the infected pockets. One end of the bowel is brought up to the skin as a stoma where the bowel content comes into the bag. This, in most instances, can be reversed later, if the inflammation is not too severe and the bowel can be joined back together.
Bleeding:
Where a severe bleeding episode has occurred an emergency blood transfusion may be required. Bleeding stops without treatment in 8 in 10 people who experience a severe bleeding episode. In those who do not stop bleeding a special x-ray test can be used to identify the site of bleeding and stop it in the majority of cases. Various endoscope techniques can also be used so ask your doctor or nurse about what treatment is advised.

Myths
If you look on the Internet you will likely still see older information about diverticular disease development, you may also see wrong advice about avoiding certain foods. You may have read that with a diagnosis of diverticular disease you need to avoid sources of tough fibre such as:
- Seeds
- Nuts
- Popcorn
- Fruit skins
It was previously felt that these foods were likely to lodge in the diverticula and cause diverticular disease and diverticulitis. This is not the case so these foods can be consumed as part of a healthy balanced diet.
What about diverticulitis?
There has been a review into whether reducing fibre intake during acute diverticulitis is helpful in reducing hospital stay, digestive symptoms or recurrence of diverticulitis. No information was found that following low fibre or low residue diets was more helpful for people with uncomplicated diverticulitis than a more liberalised (typical) diet.
There is no evidence that fibre modification is helpful in treating uncomplicated diverticulitis. Advice may however be different when complications of diverticulitis occur for example fistulas, abscesses, perforation, bowel blockages or after surgery to the bowel. Your doctor or dietitian can provide further advice as needed.
There is no evidence that probiotics (good bacteria) are helpful in treating episodes of diverticulitis.
Support
What to ask your doctor?
These are some useful questions you can ask your doctor:
- Has my colonoscopy/CT scan ruled out any other conditions?
- Are there any issues of potential concern in my large bowel?
- Would you refer me to a dietitian for further help with my diet?
- What monitoring or follow up will I be offered?
- When will antibiotics be considered when treating my diverticulitis and when should I seek further advice?
Where can I get more information about treatment?
The National Institute of Health and Care Excellence (NICE) make evidence based recommendations on a wide range of topics in health, public health and social care. They recommend the most effective ways to prevent and manage specific conditions and to improve health and manage medicines in different settings.
How can I be involved in research into diverticular disease?
It is important that research continues into the causes and treatments for diverticular disease. If you are interested in taking part in research then contact Guts UK or the National Institute of Health Research (NIHR) website. You can donate to Guts UK and join our community.
References are available on request. Contact Guts UK.
What are NICE Guidelines?
The National Institute of Health and Clinical Excellence make evidence-based recommendations on a wide range of topics in health, public health and social care. They recommend the most effective ways to prevent and manage specific conditions and to improve health and manage medicines in different settings. You can find their guidelines on diverticular disease here.
Research
Guts UK is delighted to announce we’ll soon begin a ‘Priority Setting Partnership’ (PSP) into diverticular disease. This will give you the opportunity to have your say and tell us what research you’d like to see into diverticular disease. Together with healthcare professionals, other patients and family members, you can decide the top 10 priorities for research into diverticular disease. Read more and sign up for updates here.
It is important that robust research continues into the causes and treatments for diverticular disease. Guts UK is the only UK charity funding research into the digestive system from top to tail. We’re proud to produce patient information for diverticular disease and we’re here to help, please contact us with any questions.
 ABOUT US:
ABOUT US:
Guts UK’s vision is of a world where digestive diseases are better understood, better treated and where everyone who lives with one gets the support they need. We fund life-saving research into diseases of the gut, liver and pancreas.
Champion our cause; help us fight digestive diseases and change the lives of millions of people in the UK by supporting our work today.