Anal Fistulas
Print this pageOverview
This factsheet is about anal fistulas
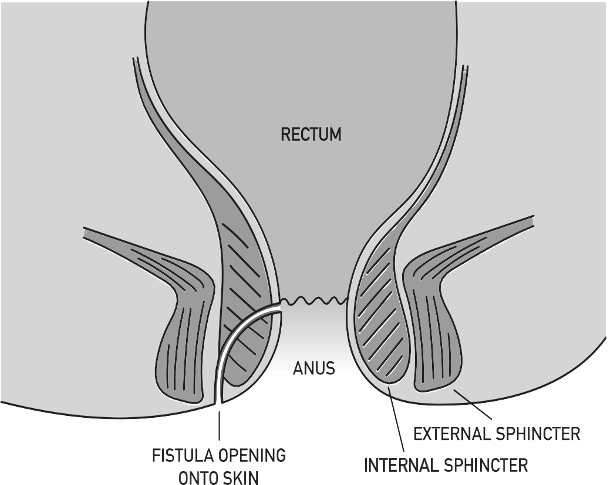
An anal fistula is a channel that develops between the end of the bowel and the skin near the anus.
Causes
What is the cause of anal fistulas?
Anal fistulas are normally caused by an infection around the anus. The infection causes a build-up of pus (abscess) that leaves a channel behind when it has drained away. The channel (fistula) persists causing symptoms of pain and irritation, smelly discharge from near the anus that can look like pus or blood, and painful swellings (abscesses). The end of the fistula may be visible as a hole or small lump in the skin close to the anus. More rarely a fistula develops due to other medical conditions such as Crohn’s disease (a type of inflammatory bowel disease), hidradenitis suppurativa (a skin condition), infection with tuberculosis (TB) or HIV, or following radiotherapy or chemotherapy cancer treatment.
DIAGNOSIS
HOW ARE FISTULAS DIAGNOSED?
Your doctor will examine you and ask about your symptoms. Some fistulas can be easy to see but others might need to be identified by using an MRI or specialist ultrasound scan to see where the tract is.
HOW CAN fistulas AFFECT YOU?
An anal infection or abscess is quite common and does not always lead to a fistula. Fistulas may result in pain, itching and a smelly discharge. You might have a painful swelling near your anus.
Unfortunately, once a fistula has developed, it usually requires surgery as it is unlikely to heal on its own if left untreated.
Treatment
WHAT TREATMENT IS AVAILABLE FOR ANAL FISTULAS?

The chosen treatment depends on the severity of your symptoms, their medical history and the type of fistula. Each fistula is different in terms of the path it takes through the muscles in the anus (sphincter muscles). The muscles are in two layers (internal and external) and a fistula can travel through or between these layers. Some complex fistulas can have side branches as well as one main tract.
Surgery allows all the infection to drain while at the same time avoiding damage to the delicate sphincter muscles around the anus as these muscles are important for maintaining bowel control (continence).
It is important to realise that a fistula is often difficult to treat. More than one operation is commonly needed to get a fistula to heal. Sometimes a fistula can be so difficult to heal that the focus of treatment is to allow them to drain well to improve symptoms.
- Fistulotomy: This involves making a cut along the length of the fistula it allows all infection to drain and leaves an open wound that takes 1 to 2 months to heal completely. However, it does involve cutting some of the sphincter muscle and if too much muscle is damaged it can result in incontinence. It is the most commonly performed operation for anal fistula, but it is only recommended for those people whose fistula does not involve too much sphincter muscle.
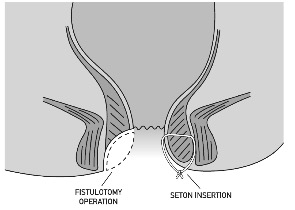
- Seton: A seton is a stitch that is threaded along the fistula. This does not allow the fistula to heal but it does allow some of the infection to drain easily. A seton controls symptoms and allows the fistula to stabilise prior to planning further operations. Setons are often used for fistulas that involve too much muscle to be treated by a fistulotomy operation. Some fistulas require several operations to get them to heal and this usually involves a combination of seton operations and other secondary options such as LIFT, advancement flap, paste or VAAFT (see below).
- LIFT: LIFT stands for ‘litigation of the inter-sphincteric fistula tract”. This operation making a cut around the anus and finding the fistula between the different layers of sphincter muscle. Once found the fistula is tied off. This operation can be effective but is not suitable for all types of fistula.
- Advancement Flap: For some fistula, the lining of the lower bowel (inside the anus) can be lifted up, as a flap, and used to cover the opening of the fistula. Like the LIFT procedure, an advancement flap can be effective and the risk of damage to the sphincter muscles is low.
- Plugs and paste: A plug is a thin strip of material made from collagen that is pulled into the fistula to block and plug the space. Similarly, a paste made from collagen can be squeezed into the fistula tract to block it. It is thought that these techniques can be effective in some cases but probably not those fistulas that contain side branches. Again, the risk of damage to the sphincter muscle is low.
- VAAFT: This stands for video assisted anal fistula treatment and involves passing a very small camera along the path of the fistula. This allows the path to be seen (including side any branches) and washes out all the infective material. Cautery (heat treatment) is then performed to clean and close the fistula. The procedure can be repeated in the future if necessary and the risk of damage to the sphincter muscle is low.
- Laser treatment / Radiofrequency ablation (RFA): A wire can be passed along the path of the fistula that delivers heat treatment from either a laser or an electrical current at the frequency of radio waves. This heat treatment attempts to clean and close the fistula tract.
- The operation: Anal fistula operations are usually performed as a day case procedure under a brief general anaesthetic, or a spinal anaesthetic (a needle into the back.) You may have a pre-assessment appointment before the operation to ensure that you are fit enough for the procedure. Just before the operation, you may be given an enema (some liquid inserted into the anus to empty the lower bowel.)

Following the operation, you may have a dressing (particularly if you have had a fistulotomy operation.) You will be monitored for a few hours in recovery before being discharged home. You will be given some painkillers to take home with you. The painkiller codeine can cause constipation so you may be given some laxatives with this.
- Operation risks: All operations carry some degree of risk. It is possible that there can be bleeding or bruising around the operation site. Any cut that is made can get infected. Even with operations where there is great care not to damage the sphincter muscle one in 10 people may experience some degree of incontinence to gas and liquid (wet wind.)
- After the operation: After a few days provided you feel well and the pain is controlled, you should be able to resume normal activities including driving, heavy lifting and going back to work. If you have dressings, you may need these to be changed or removed by the nurse at your GP practice.
Some fistulas may need several operations to allow them to fully heal. You may be booked for a planned operation (especially if your operation involved putting a seton along the fistula) or you may be seen in the clinic.
Support
HOW CAN FISTULAS AFFECT ME OVER TIME?
In the long term a few people may experience problems with continence. If you are experiencing problems then most local NHS services will have a continence service, which can be a very useful service to approach to seek advice in managing symptoms. Most continence services do accept a referral from the individual (you don’t always need to ask your GP or consultant for a referral) you can call the service yourself and request advice.
Bladder and Bowel UK give independent advice on products that help bowel continence issues, and they can also provide a ‘can’t wait card’ that can help with toilet access when going out in the community.
You might find the Great British Toilet Map useful.
WHAT TO ASK YOUR DOCTOR?
- What type of surgery is going to be best for my fistula?
- Do I need any additional tests to check what has caused the fistula?
- Will my fistula re-occur?
- Do you have contact details for the local continence service?
 WHAT WE DO:
WHAT WE DO:
Guts UK’s vision is of a world where digestive diseases are better understood, better treated and where everyone who lives with one gets the support they need. We fund life-saving research into diseases of the gut, liver and pancreas.
We hope our expert, evidence-based, reliable information helped you today. Please consider donating to Guts UK today, so we can continue to help the millions of others in the UK just like you. Let’s get to grips with guts.





