Chronic pancreatitis
Download printable versionOverview
This factsheet is about chronic pancreatitis
Chronic pancreatitis is a long-standing inflammation of the pancreas. Although the condition is rare, between 6,000 and 12,000 people in the UK are given a new diagnosis every year. Men are more likely than women to develop chronic pancreatitis, and those in their middle to late years are most susceptible.
What is the pancreas?
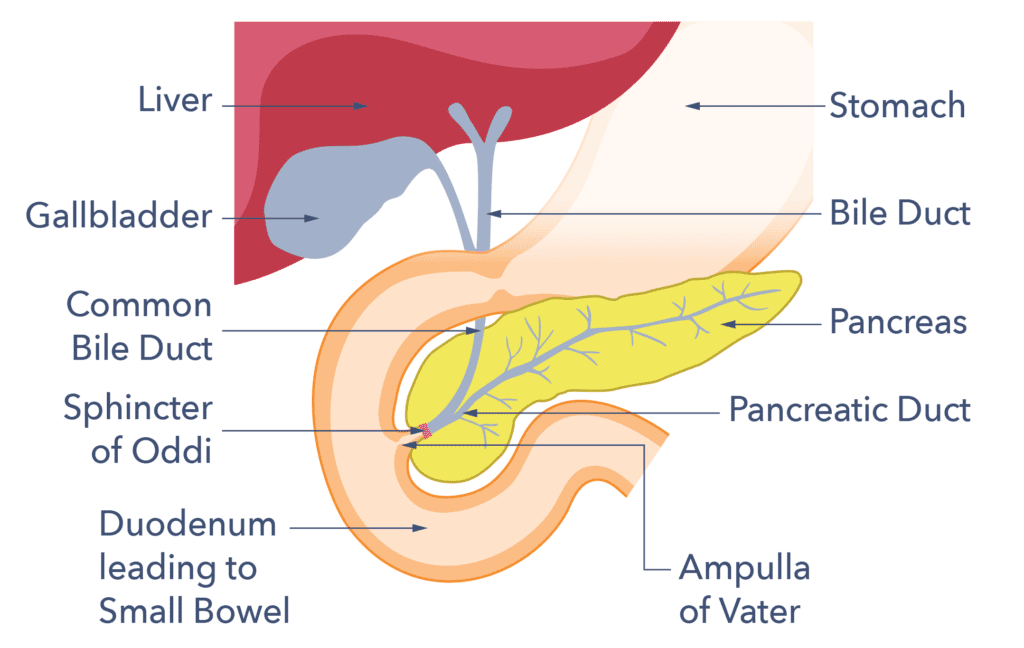
The pancreas is a gland that lies in the upper half of the belly (abdomen) behind the stomach and in front of the spine. It is roughly 25 cm (nine inches) long and salmon pink in colour. At its widest point, about the thickness of your wrist. Our ability to properly digest food depends on the pancreas. It does this in two main ways.
1) The pancreas makes juices that balance the acid made in the stomach. The juice contains digestive enzymes to break down the protein, starch and fat content of our food into smaller pieces. Smaller pieces are easier to absorb (soak up, like a sponge) into our body. Pancreatic juice flows into the upper small bowel (the duodenum) and mixes with food and bile to help digest the food we eat. Bile is a substance made in the liver to help digest fats.
2) The other role of the pancreas is to make hormones (chemicals), including insulin. Insulin helps sugars enter body cells from the blood to use for energy and increase overall energy stores in the body. This role is carried out by specialised cells embedded in the pancreas.
What is chronic pancreatitis?
Chronic pancreatitis is a long-standing inflammation of the pancreas. The normal pancreas is soft with a smooth surface. In chronic pancreatitis the normal pancreas cells are steadily lost due to damage caused by the inflammation. Scar tissue (fibrosis) forms in these inflamed areas, making the pancreas irregular and hard. In the late stages of the disease, calcium is deposited in the scarred areas. The bile ducts (tubes which transport digestive juices to the intestine) may also become irregular with narrowings (strictures) and ballooned (dilated) segments. Plugs of protein may collect in the ducts and eventually large stones may form. Pseudocysts (fluid-filled cavities) may also be found around the pancreas.
Chronic pancreatitis is rare. In the UK between 6,000 and 12,000 people are given a new diagnosis every year. These figures are probably an underestimate as it can be difficult to diagnose. As the disease progresses or as problems arise, the diagnosis gets easier. For people with acute pancreatitis 8 out of 100 people may go on to develop chronic pancreatitis. Men are more likely than women to develop chronic pancreatitis, and those in their middle to late years are most susceptible.
Causes
What are the causes of chronic pancreatitis?
The causes of chronic pancreatitis varys greatly. In most people with chronic pancreatitis there is probably a combination of family (genetic) and environmental factors.
The most frequent cause of chronic pancreatitis is drinking too much alcohol (about 7 in 10 people with chronic pancreatitis). Smoking tobacco is recognised as harmful to the pancreas as well. Even among smokers and/or people who drink too much alcohol, chronic pancreatitis is uncommon. Once chronic pancreatitis is established however, it is important to give up tobacco and alcohol to prevent progression of the disease. Stopping smoking and alcohol also has added benefits of reducing complications and improving painful symptoms.
High levels of fats (triglycerides) or calcium in the blood are also known to cause chronic pancreatitis. Some prescribed medications can cause chronic pancreatitis. Examples include azathioprine and sodium valporate.

Some people who have specific genes are prone to develop chronic pancreatitis. The most common is the cystic fibrosis gene. Cystic fibrosis is also the commonest cause of chronic pancreatitis in children. Hereditary pancreatitis is a very rare genetic disease which runs in families. For the others, it’s likely that a combination of small genetic changes results in certain people having a higher risk of developing chronic pancreatitis.
Autoimmune pancreatitis occurs when the body’s own immune system attacks the pancreas. This disorder may be linked to other autoimmune diseases, such as primary biliary cirrhosis and inflammatory bowel disease. But it is also likely to have a genetic background. Pancreatic divisum is a difference in the way that tubes leading from the pancreas develop in the foetus.
Pancreas divisum happens in 1 in 10 people. This difference in structure can increase a person’s risk of having acute pancreatitis and over time the risk of developing chronic pancreatitis. Most people with pancreatic divisum do not experience any problems. Bile duct obstructions caused by tumours, stones or scarring from trauma/injury can also cause chronic pancreatitis.
There is an association with gallstones. If an episode of acute gallstone pancreatitis is very severe and results in lasting damage this can be a cause of chronic pancreatitis. This can also happen with severe and recurrent episodes of acute pancreatitis, whatever the cause. Unfortunately, in up to 3 out of 10 people with the condition, the cause cannot be identified, despite thorough investigation. This is known as “idiopathic” chronic pancreatitis.
Diagnosis
How is chronic pancreatitis diagnosed?
Chronic pancreatitis is hard to diagnose. This is because it is rare and the symptoms overlap with other more common conditions, such as Irritable Bowel Syndrome (IBS). In fact the average GP practice in the UK would see less than one newly diagnosed person with chronic pancreatitis per year. Investigation aims to show abnormalities in the structure of the pancreas and/or how the pancreas works. A specialist gastroenterologist or specialist liver, biliary and pancreas surgeon usually supervises a person’s care.
Unfortunately, there is no single test for chronic pancreatitis at this time, and many pancreatic cells can be damaged before abnormalities on tests show up. The pancreas’s production of digestive enzymes and the number of insulin-producing cells can become depleted long before symptoms of poor digestion or diabetes appear. Once the damage and scarring advances and becomes more severe the pancreas damage may be detected by blood tests or scans. However, by this time complications like diabetes may already be present.

Investigations involve scans, such as CT and MRI scans which give the best pictures of the pancreas. But ultrasound scans may also be used. If extra information is needed, an endoscope may be used. An endoscope is a thin wire, with a camera that is inserted into the digestive tract through the mouth to the top of the small bowel. The endoscope is used to get internal ultrasound pictures (EUS, or an endoscopic ultrasound scan). This is where the ultrasound device is attached to the end of the endoscope. This gives a very accurate picture of the pancreas and the tubes leading from the gallbladder and pancreas.
The simplest test of the function of the pancreas (how good it is at producing digestive juices) is the faecal elastase test. This test is performed on a small sample of poo. But, this is not always reliable. MRI can assess the volume of digestive juice produced by the pancreas after an injection of a hormone called secretin. The best current method however is a mixed triglyceride breath test, but this is not available everywhere.
Blood tests to look for vitamin and mineral deficiencies can also support a diagnosis of pancreatic exocrine insufficiency (PEI) and chronic pancreatitis.
Symptoms
What are the symptoms of chronic pancreatitis?
The major symptoms of chronic pancreatitis are:
- Pain
- Nausea
- Vomiting
- Diarrhoea
- Weight loss
- Fatigue
Some people with chronic pancreatitis have only one or two of these symptoms. Symptoms of diabetes may happen late in the disease.
The pain of chronic pancreatitis can range from mild to severe and is felt across the upper abdomen. Chronic pancreatitis causes upper abdominal pain (just below the ribs) that can range in intensity from mild to severe. Additionally, the pain could radiate to the back. Some people get relief from crouching forwards. Eating can make the pain worse. The pain may be constant, or it may come and go. Some people also get attacks of acute pancreatitis or flares in their painful symptoms. Painless chronic pancreatitis occurs in 1 in 10 people with chronic pancreatitis. This is particularly true of people with idiopathic and genetic causes of their pancreatitis. This means most people with chronic pancreatitis will experience pain.

The cause of pain in chronic pancreatitis is debated. Increased pressure in obstructed ducts may be a factor. There is evidence of over-growth and increased firing of nerves in the pancreas itself. The brain may also become sensitised to pain signals from the pancreas, forming a pain-loop.
There may also be more generalised abdominal (belly) discomfort, feeling sick (nausea) and bloating, which can make eating difficult. Diarrhoea in chronic pancreatitis is caused by poor digestion of food. The classical description is large volumes of loose or runny pale, floating poo with a particularly strong smell. An oily film may be present, the poo is hard to flush away and stains the toilet bowl. Many people learn that fatty foods worsen this symptom, but avoiding fat contributes to weight loss and malnutrition. Weight loss happens partly through poor absorption of food and partly through loss of appetite or food-avoidance due to these symptoms. Many people with chronic pancreatitis feel unwell in themselves, lethargic and fatigued. Some also suffer side-effects from pain-killing drugs.
As with any chronic condition, sufferers may experience psychological symptoms such as depression and relationship problems. The physical and psychological burden can also affect a person’s ability to work and consequently, has an impact on their finances. Any severe or new symptoms should not be ignored. Severe or new symptoms may indicate a disease complication that needs specialised treatment.
How can chronic pancreatitis affect you?
Chronic pancreatitis is a complex disease that can have a huge impact on quality of life. It is vital to give up both smoking and alcohol even if they are not the primary causes of your pancreatitis. Both are known to make the disease worse.
Diabetes
The number of people with chronic pancreatitis who are diagnosed with diabetes increases over time. 25 people in 100 to 80 people in 100 will develop diabetes within 10 to 20 years. Symptoms which should be discussed with your doctor include:
- Unintentional weight loss
- Feeling very thirsty
- Peeing more frequently than normal, particularly at night
- Craving sugary foods and drinks
Other symptoms might include tiredness and blurred vision. People with chronic pancreatitis should be monitored for the development of diabetes every six months even if they have no symptoms of diabetes. This can be done using a simple blood test known as a HbA1c.
Pancreatic exocrine insufficiency (PEI)
8 in 10 people with chronic pancreatitis will develop pancreatic exocrine insufficiency (PEI) over time. This is poor absorption of food due to a lack of digestive enzymes resulting from the damaged pancreas being unable to produce enough. It is more likely to occur when necrosis (or death) of pancreatic tissue has occurred. Plus, PEI is also more likely for people who have been drinking alcohol in excessive amounts. Symptoms include:
- Loose or runny pale, smelly stools (poo) which may float in the toilet and are difficult to flush away (called steatorrhoea)
- Bloating
- Belly (abdominal) pain
- Weight loss
Ask your doctor if this applies to you. People with a diagnosis of chronic pancreatitis should be monitored for the development of PEI using a yearly faecal elastase test. This test is advised even if their bowel habit is normal.
Osteoporosis
People with chronic pancreatitis can also be at risk of weakened bones (osteoporosis). 2 in 3 people with chronic pancreatitis can develop weakened bones over time. This can result in broken bones. A bone scan (DEXA scan) to assess bone density should be performed every two years in people with chronic pancreatitis.
Vitamin D deficiency
People with chronic pancreatitis are prone to vitamin D deficiency and may require prescribed vitamin D supplementation. People with darker skin tones may need to take vitamin D more regularly. This is because they may be less likely to be able to produce enough through the skin. Talk to your doctor if this applies to you.
What are the main complications of chronic pancreatitis?
The two main complications of chronic pancreatitis are diabetes and PEI.
Diabetes related to pancreatitis is called Type 3c diabetes. It occurs because of damage to the pancreatic cells that produce insulin. The pancreas cells produce many different hormones which contribute to the control of sugar levels. Type 3c diabetes may be difficult to control. The usual treatment is diabetic medication in the form of tablets such as Metformin. Many people with chronic pancreatitis will need insulin injections and specialist diabetes service advice. Insulin can help patients put weight and muscle back on. The National Institute of Health and Care Excellence (NICE) has indicated a need for research in this area.
PEI can cause maldigestion, weight loss, vitamin deficiencies and lead to malnutrition. The treatment is pancreatic exocrine replacement therapy (PERT) and a healthy balanced diet.

Swelling and scarring of the pancreas occasionally leads to obstruction of the pancreas itself. The bile duct or the duodenum (the part of the small bowel which drains the stomach) can be blocked. Obstruction of the ducts is usually treated by putting stents, (small internal drainage tubes) through the obstruction using an endoscope (ERCP). Sometimes surgical operations are also used. NICE has advised that more research is needed in this area. A blockage of the top of the small bowel (duodenum) is rare and may need an operation to bypass the blockage. Pancreatic pseudocysts can form around the pancreas causing pain and symptoms of nausea and vomiting. Pseudocysts may resolve on their own or may need draining by placement of a stent from the stomach to the cyst (a cystgastrostomy). This is usually performed with an endoscope. This procedure is done in specialist pancreas centres.
Some people with chronic pancreatitis also have episodes of acute pancreatitis and any new or worsening pain requires investigation.
People may worry about whether they will die from chronic pancreatitis. The likelihood is low. Research suggests most people die from other causes such as cancer or heart disease. Drinking alcohol and smoking are factors that you can try to stop in order to reduce your risk of these diseases. As these factors also risk worsening chronic pancreatitis, it is a good idea to stop if this applies to you.
If you have chronic pancreatitis, you have an increased risk of developing pancreatic cancer. This risk is particularly high if you have hereditary pancreatitis. Your pancreas team will monitor your condition and advise you if they judge that you should be investigated for cancer. People with hereditary pancreatitis may be asked to take part in trials looking at ways of detecting cancer early.
Chronic pancreatitis can complicate other illnesses with genetic components. Examples are some hyperlipidaemias (high blood fats), high blood calcium, kidney disease and inflammatory bowel disease.
Treatments
How can chronic pancreatitis be treated?
A multidisciplinary team (MDT) approach to care is required. This includes general practitioners (GP), pancreas specialists in the hospital, specialist nurses and dietitians. Some people need access to specialist care for treatment of complications, including diabetes, pain and psychological services. Unfortunately, there are no curative treatments for chronic pancreatitis. The aim is to prevent further damage to the pancreas to help:
- Slow disease progression
- Control symptoms
- Reduce complications
- Improve quality of life
It is vital to give up both smoking and alcohol even if they are not the primary causes of your pancreatitis. Both are known to make the disease worse. Specialist support is available. Ask your GP what services are available in your area.
Pain is treated using a step-up approach with oral pain killers. The minimum effective treatment is used at any time to give pain-relief while minimising side-effects. If ‘simple’ pain-killers such as paracetamol are ineffective, stronger drugs may be needed.
Opioid pain medicines are excellent at controlling short-term pain, but are addictive, cause constipation and may cause pain with long-term use. Pain-modifying drugs which change the way our nerves and brain interpret pain-signals (neuromodulators) may give better long-term control. Examples are amitriptyline, gabapentin or pregabalin.

Using opioid-based pain medicine for short term relief of pain flares, alongside neuromodulator drugs, may be needed for some people. Each situation must be decided by a conversation with your doctor or specialist nurse. The aim is to enable the person to attain a reasonable quality of life, whilst managing the pain as well as possible. The hospital pain management team can also be involved in treatment. Your GP can refer you. The National Institute for Health and Care Excellence (NICE) has advised that more research is needed in this area.
Some people with severe pain which is not controlled by pain-killing medicines benefit from injections to block the nerves coming from the pancreas. This is only done through the skin or via an endoscope and should only be done after careful consideration in specialist centres.
Non-surgical procedures are a part of pain treatment for some people. People with stones in the main pancreas duct may get relief if they are removed using an endoscopic procedure (ERCP). Stents can also be inserted into narrowed ducts to help with pain in some patients. It is sometimes also possible to break up stones using shock wave lithotripsy (ESWL). Occasionally, bile duct strictures (narrowing) arise due to chronic pancreatitis and can cause jaundice. These can also be treated using ERCP to place stents into the bile duct. Endoscopic treatment to treat other complications like large pseudocysts can also help improve pain. This treatment must be performed by an experienced practitioner.
Pancreatic exocrine insufficiency (PEI) is treated with pancreatic enzymes known as Pancreatic Enzyme Replacement Therapy (PERT). They contain the pancreatic enzymes to help replace the enzymes a normal pancreas would produce. These are given in tablet or powder form. They are taken spread throughout every meal. They are also to be taken with snacks containing fats and with nutritious drinks such as milk. They work with your food, not with your body.
An acid-reducing PPI (proton-pump inhibitor) medicine may also help. There are several different ones including omeprazole, lansoprazole and esomeprazole. In PEI the top of the small bowel is more acidic than usual because the pancreas makes less bicarbonate. Bicarbonate is a substance which neutralises stomach acid. Pancreatic enzymes don’t work in an acidic environment, so PERT capsules have a coating which stops the enzymes being released into acid. Guts UK have a separate information booklet on PEI.
Most people with chronic pancreatitis should eat a normal balanced diet, although some find it easier to have more smaller meals throughout the day. Dietary restrictions can be harmful. It is important to note that low fat diets can mask PEI symptoms. It is not an appropriate treatment to use for most people with chronic pancreatitis. Prescription of digestive enzymes when needed is the correct treatment to allow a normal diet to be consumed. The aim of enzyme therapy is to allow digestion of normal meals without symptoms, and to regain weight.
A rare exception to this advice is when someone has been diagnosed with an inherited (genetic) problem with very high blood cholesterol or triglyceride levels that can cause pancreatitis. This will be explained to you by your specialist team. Some people may need help to meet their nutritional needs using feeding tubes if they are unable to meet them by eating normally.
Every person with chronic pancreatitis should see a specialist qualified dietitian, who is a vital part of the chronic pancreatitis team. Other ‘nutritional therapists’ should be avoided. They have variable training and may give poor or dangerous advice. The type of digestive enzymes that are promoted by health food shops and nutritional therapists contain tiny amounts of enzymes. They are not likely to be effective. The only effective enzymes are those prescribed by a doctor, or non-medical prescribers such as a specialist nurse or prescribing dietitian. Effective use of digestive enzymes can help reduce digestive symptoms and pain. Talk to your doctor if you feel you have PEI or if you need a review of your prescribed dose.
Many people with chronic pancreatitis develop secondary or Type 3c diabetes and are wrongly diagnosed with Type 2 diabetes. This leads to inadequate treatment. For people with Type 3c diabetes the treatment includes medications that regulate blood sugar control, but many people need to take insulin. Type 3c diabetes can be difficult to control and when this occurs people are usually referred to a specialist diabetes service.

Surgery is only offered in special pancreas centres after careful investigation and discussion. Operations to drain dilated ducts and remove inflamed tissue may relieve pain in some people. Occasionally the whole pancreas is removed (total pancreatectomy). This however causes severe diabetes. If the pancreas cells which make insulin are transplanted back, this is called total pancreatectomy with islet auto-transplantation, TPIAT, or autologous pancreatic islet cell transplantation (APICT). Where this has been done the diabetes may be less severe. This operation is reserved for people whose pancreas still produces insulin. This is available for people who are fit enough for surgery with hereditary pancreatitis and those people with acquired chronic pancreatitis. There are NHS criteria for referral. This can be discussed this with your doctor.
The stress of living with a painful chronic illness can lead to anxiety and depression. People with pancreatitis may struggle with isolation, relationship problems, addiction, unemployment, and the financial pressures this brings. Treatment can include psychological therapies such as alcohol cessation support, cognitive behavioural therapy, personal counselling and mindfulness delivered by specialist psychological services.
The NICE guideline for pancreatitis recommends that people with chronic pancreatitis are offered monitoring of their pancreatic exocrine function and of their nutritional status at least every 12 months. This is more frequent (every six months) in under 16’s. This should be done by clinical and biochemical assessment, to be agreed with a specialist pancreatic centre. This usually involves blood tests to look for nutritional deficiencies, a faecal elastase stool test and a review of your symptoms by a doctor, nurse or dietitian.
Support
What support is available?
You will be cared for by your GP practice together with a specialist pancreas team at your local hospital. Your local pancreas team may refer you to a specialist pancreas centre if you need special investigations or an operation. Chronic pancreatitis is a complex disease that can have a huge impact on quality of life. For people suffering with chronic pain, a referral to a local chronic pain service can help. Clinical psychology is also available via the NHS to help people cope psychologically with the effects of chronic pancreatitis. You can also read tips and suggestions from other chronic pancreatitis patients on how to manage the disease. Contact Guts UK Charity for help and information.
New NICE Guidelines on pancreatitis
The new NICE Guidelines on pancreatitis aim to improve the quality of care, information provision and support for people with chronic pancreatitis. The guidelines have a section on information to the public, explaining the care that patients should expect.
> Read our tips & suggestions for pancreatitis patientsResearch
What additional research is needed?
 There is a need for research into every aspect of chronic pancreatitis, from the laboratory to clinical practice. The last 20 years have seen major advances in our understanding of the mechanisms of damage to the pancreas in laboratory models, but these are incomplete and have not yet produced improvements for patients. NICE has recommended research into pain management, the treatment of bile-duct obstruction, and insulin therapy in Type 3c diabetes.
There is a need for research into every aspect of chronic pancreatitis, from the laboratory to clinical practice. The last 20 years have seen major advances in our understanding of the mechanisms of damage to the pancreas in laboratory models, but these are incomplete and have not yet produced improvements for patients. NICE has recommended research into pain management, the treatment of bile-duct obstruction, and insulin therapy in Type 3c diabetes.
Guts UK Charity, the British Society of Gastroenterology and the Pancreatic Society of Great Britain and Ireland have jointly funded a James Lind Alliance Priority Setting Partnership (JLA PSP). This is a collaboration of patients, carers, healthcare professionals and researchers to produce a list of the top ten unanswered research questions for pancreatitis. The results of this study can be found on the on the research pancreatitis PSP webpage. The new NICE guidelines on pancreatitis have a section with recommendations for research.
Guts UK Charity is proud to fund pancreatitis research. We are the only UK charity funding a research fellowship into pancreatitis. We are dedicated to find an effective treatment, or a cure for this condition.
You are through to the right place:
 Pancreatitis is a priority area for Guts UK. We fund research into pancreatitis that has the potential to change and save lives. Our Kranky Panky Pancreatitis Awareness Campaign each November builds a community of those affected by pancreatitis, comforted in knowing they’re not alone. Our expert information allows those with pancreatitis to take control of their health, and make informed decisions.
Pancreatitis is a priority area for Guts UK. We fund research into pancreatitis that has the potential to change and save lives. Our Kranky Panky Pancreatitis Awareness Campaign each November builds a community of those affected by pancreatitis, comforted in knowing they’re not alone. Our expert information allows those with pancreatitis to take control of their health, and make informed decisions.
We believe it’s time the UK got to grips with guts. Your support takes us one step closer. Donate today.